As health systems globally continue to be severely strained by the COVID pandemic, it’s important to remember that other diseases, such as cancer, haven’t learned to keep their social distance—they continue to proliferate. The good news is that many cancers are now highly treatable with the help of solutions like radiation therapy. Approximately 50% of all cancer patients will receive radiation treatment over the course of their illness, with one study approximating that radiation comprises 40% of curative treatment regimens.[1] By identifying the challenges that the science of radiation oncology faces today, we’ll be better equipped to formulate solutions and even more effective treatment tomorrow.
The Treatment Plan Creation Catch-22
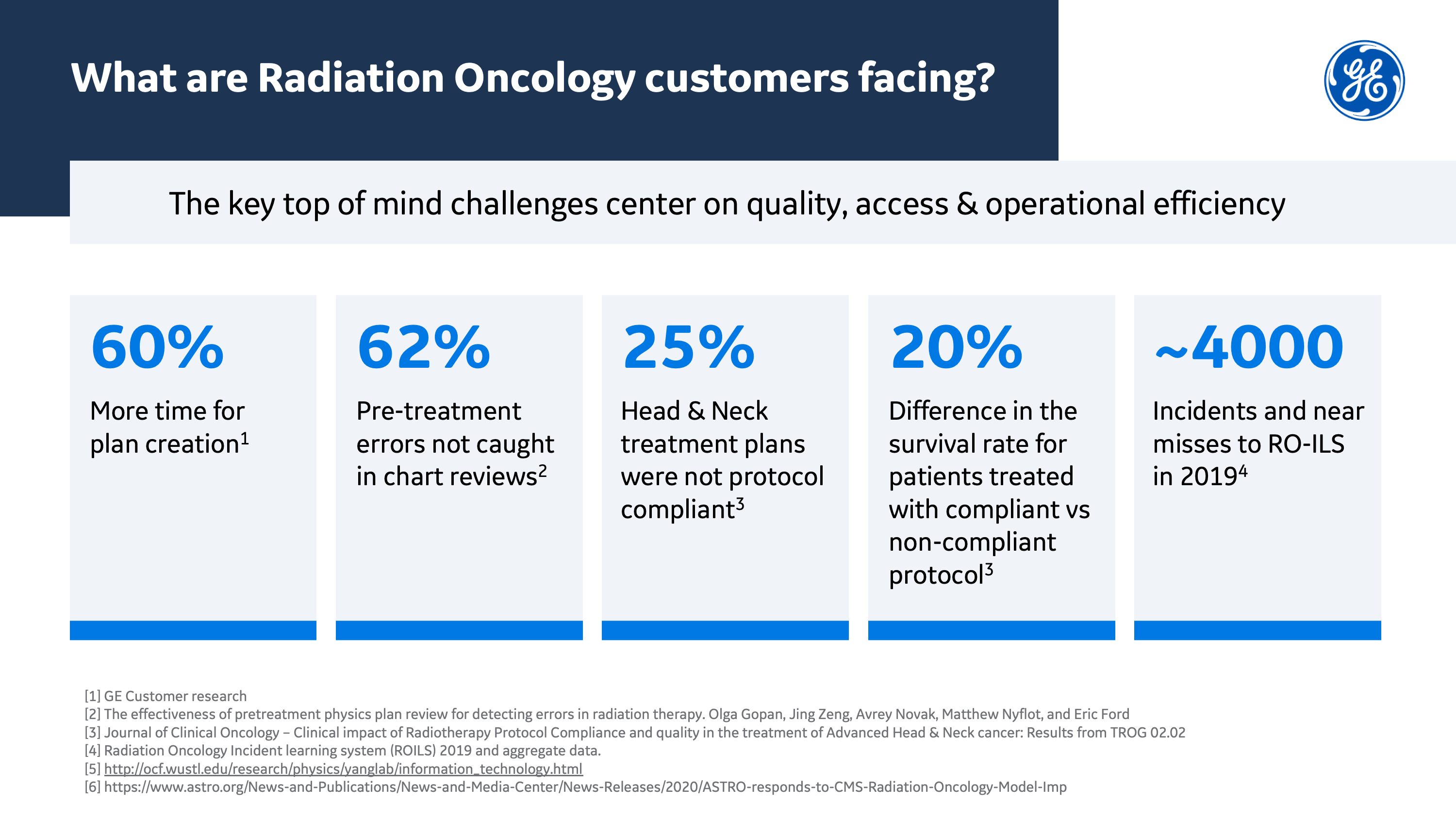
Studies have shown that most errors that occur during radiation oncology treatment originate in the planning stage of treatment. One study, Effectiveness of pretreatment physics plan review for detecting errors in radiation therapy, analyzed 522 potentially severe or critical near-miss events within an institutional incident learning system collected over three years. Of these 522 events, 356 originated at a workflow point before the pretreatment physics plan review. Clearly, treatment plan review is a crucial safety measure that can detect a high percentage of errors.[2]
Radiation solutions like intensity-modulated radiation therapy (IMRT), a highly effective cancer treatment that has the opportunity to maximize the treatment of cancers with minimal toxicity to normal organs, require not only knowledge and experience, but also one thing physicians are short on, particularly in the COVID-19 era: time.[3]
Key to the proliferation of errors in the planning stage of treatment is the fact that clinicians are already suffering from data overload. One RO-ILS (Radiation Oncology Incident Learning System) case study suggests multiple follow-up measures to address the factors that might contribute to an overly-busy clinic, including guidelines that involve slowing down the pace of treatment plan creation.[4] The authors suggest that a certain number of days should be allocated for each step in the process, and if the timeline is not met, a proactive delay in the onset of treatment should be implemented. The case study concludes that staff must be allowed an appropriate amount of time to complete a treatment plan and related quality assurance (QA).
Going forward, medical device integration (MDI) will be key when it comes to enabling physicians to make accurate, evidence-based decisions quickly. When doctors have seamless access to the continuous stream of data that various devices supply to electronic medical records (EMR), the administrative burden that currently falls on clinicians will be reduced, allowing them to give more hands-on medical care. While the automation of data flow that’s necessary for MDI to be achieved still requires significant improvement, the benefits that come from achieving that interoperability make it well worth the effort.[5]
Optimizing the Pretreatment Plan Review
Progressively sophisticated medical devices are creating more data, increasing the need for interoperable healthcare systems that can break down data silos so data from disparate sources, including medical devices, platforms, and software, can communicate and cooperate.[6]
From the previously mentioned study, Effectiveness of pretreatment physics plan review, it was determined that of the 356 events located in the institutional database, 180/356 (51%) were detected or could have been detected by the pretreatment physics plan review. Of these events, 125 passed through the physics review; however, only 47/125 (38%) were actually detected at the review.[7] Interoperable systems could assist in automatically assessing some portions of the review, allowing physicians to spend more time on the complex, nuanced portions of the review. At this point, comprehensive interoperable systems that can reliably supplement physician review have yet to be created.
The errors within these pretreatment plans that led to adverse events were evaluated to determine if they could be caught and corrected sans physician review with automated programming. A similar analysis was carried out on 81 events from the international SAFRON radiation oncology incident learning system. Of the 81 events from the SAFRON database, 66/81 (81%) were potentially detectable by the pretreatment physics plan review. Based on this analysis, software-based plan checking systems, if available, would have potential effectiveness of 29% and 64% at detecting events from the institutional and SAFRON databases, respectively. Imagine if this data can be aggregated and synthesized accurately, producing actionable information—it could result in far fewer pre-treatment errors, with no additional burden put on physicians.[8]
Implementing Effective Infrastructure
Radiation therapy is a treatment that’s key in the efforts to treat head and neck cancers.[9] While technological advances have led to improved treatment outcomes and expanded implications for the use and efficacy of radiation therapy in treating head and neck cancers, radiotherapy treatment plans frequently fall prey to human error and aren’t always completely protocol compliant, resulting in substandard patient outcomes.
A study entitled Critical Impact of Radiotherapy Protocol Compliance and Quality in the Treatment of Advanced Head and Neck Cancer, published in the Journal of Clinical Oncology, reviewed the impact of radiotherapy quality on the outcome in a large international phase III trial designed to evaluate radiotherapy.[10] The Quality Assurance Review Center (QARC) performed interventional review of radiotherapy plans within the study, while the Trial Management Committee (TMC) examined radiotherapy plans and documentation for protocol compliance post-treatment. TMC review identified that 25.4% of patients in the study had noncompliant plans in which no QARC-recommended changes had been made. At secondary review, 47% of noncompliant plans (comprising 12% of plans overall) had deficiencies that resulted in a predicted major adverse impact on tumor treatment.
This study presents a compelling argument for the necessity of developing and implementing interoperational automated QA solutions. Care can’t become more democratic and accessible until workflows are dramatically streamlined and protocol compliance in treatment administration becomes the norm. For example, when the Centers for Medicare and Medicaid Services announced, in September 2020, that an advanced alternative payment model had to be implemented in radiation oncology practices on January 1st of 2021, Theodore L. DeWeese, MD, FASTRO, Chair of the ASTRO Board of Director, responded with the following statement:
"Achieving value-based care in radiation oncology that improves outcomes for cancer patients has been a longstanding goal of ASTRO. The final Radiation Oncology Model announced today by the Center for Medicare and Medicaid Innovation begins moving the specialty in that direction but fails to address many of the radiation oncology community’s key concerns…The transition to value-based payment will require significant practice changes and investments to comply with the model's requirements. ASTRO strongly urges CMS to significantly delay the start date rather than foster unnecessary chaos and burden for the practices this model is designed to support.” [11]
For high-quality care to be easily accessed by everyone, we have to create the streamlined infrastructure required to ensure that solutions, both financial and medical, can be administered in a highly effective way.
RO-ILS & The Power of Combined Resources
Human beings are fallible creatures, a fact that can’t be fixed. However, we can learn from our mistakes. In June of 2014, The American Society for Radiation Oncology and the American Association of Physicists in Medicine launched RO-ILS: Radiation Oncology Incident Learning System, a radiation oncology incident learning system and national patient safety initiative designed to provide safer, higher quality care in radiation oncology at no cost to providers or facilities.[12] The system allows internal incidents, near misses, and unsafe conditions to be tracked, reviewed, and contributed to a national database, with the hope that the collective knowledge will improve the field of radiology.
Nine out of 10 RO-ILS participants expressed that they found the program to be moderately to very valuable. Because the RO-ILS portal is web-based, this one shared system can span an entire health network, eliminating data silos. Practices can benefit from data aggregation and improved analytic capabilities by identifying unique, shared data trends across different facilities.
One RO-ILS case study highlighted the importance of adaptive planning as a key part of the radiation oncology process.[13] A common adaptive planning approach sees patients subjected to a quality assurance repeat CT (QACT) during the first 10 fractions of radiotherapy treatment. This is typically repeated two to three times over the course of radiotherapy. Improving the accuracy and precision of radiation treatments potentially reduces morbidity while improving cancer mitigation efforts. However, adaptive planning increases workload, which, as discussed above, has the potential to contribute to more errors and slow down the treatment process.
This case study calls for the design of robust, medically integrated processes that can affect efficient implementation and communication of adaptive planning.[14] An integrated solution in this area not only has the capacity to make hospital operations more efficient, but could improve patient outcomes and enhance patient safety.
The Future of Patient Safety
Adoption of RO-ILS and the number of events reported to the Patient Safety Organization (PSO) have grown steadily over the program’s initial five years. In June 2019, the program recorded 10,000 safety events in the national database; this rose to over 12,000 events by the end of the year. More recently, a portion of larger practices have abandoned their native systems in favor of utilizing RO-ILS exclusively.[15]
The typical RO-ILS process of event reporting involves discovering an event and submitting a “Submit Event” form. A Reviewer is then notified and completes protocol for investigating the event. The Reviewer then submits their event report to PSO, while a copy of the event is also sent to the national PSO database.
Data analysis of the events recorded in the PSO database is completed by Clarity PSO, as well as the Radiation Oncology Healthcare Advisory Council, a group of 12 radiation oncology professionals working across disciplines, including radiation oncologists, physicists, dosimetrists, and therapists who provide subject-matter expertise on data interpretation and reporting and suggest possible interventions.
The annual rate of therapeutic radiation incidents, defined as radiation dose not delivered as intended, with or without harm caused to the patient, has decreased from 16% to 9% over three years. While more monitoring and analysis is required before any conclusions are drawn, this trend could suggest that practices utilizing the RO-ILS system have experienced inclusive quality improvement and/or changes to clinical practice that may be related to improved safety. It appears that incidents of non-compliant protocol that result in negative events that directly impact patients are on the decline.
An article entitled Knowledge-based planning for intensity-modulated radiation therapy: A review of data-driven approaches concluded that knowledge-based planning, a data-driven approach to IMRT planning that automatically learns from high-quality clinical plans that have accumulated over the past two decades, could improve the quality and efficiency of IMRT planning. The study identified that KBP had benefits that included achieving comparable and often improved quality of IMRT planning while reducing planning time and variation in planning quality.[16]
Ultimately, data integration provides a powerful way to improve patient care for both individual patients and patient populations at large. Within hospitals, medical devices come from a multitude of vendors; to actualize the full benefit of the data they produce, hospitals need an interoperable MDI solution that converts medical device data into formats that Electronic Medical Records can both consume and synthesize.[17] This has the potential to significantly streamline care, improve cross-team collaboration and support, and alleviate the burden that data overload from disparate sources has on clinicians, allowing them to better meet patients’ needs.
REFERENCES
[1] https://www.medsci.org/v09p0193.htm#B11
[2] https://pubmed.ncbi.nlm.nih.gov/27587048/
[3] https://aapm.onlinelibrary.wiley.com/doi/10.1002/mp.13526
[4] https://preprod.astro.org/Patient-Care-and-Research/Patient-Safety/RO-ILS/Case-Study-03
[5]https://www.gehealthcare.com/article/interoperability-in-healthcare-how-medical-device-integration-is-helping-tear-down-those-walls
[6]https://www.gehealthcare.com/article/interoperability-in-healthcare-how-medical-device-integration-is-helping-tear-down-those-walls
[7] https://pubmed.ncbi.nlm.nih.gov/27587048/
[8] https://pubmed.ncbi.nlm.nih.gov/27587048/
[9] https://pubmed.ncbi.nlm.nih.gov/31378376/
[10]https://www.researchgate.net/publication/44608389_Critical_Impact_of_Radiotherapy_Protocol_Compliance_and_Quality_in_the_Treatment_of_Advanced_Head_and_Neck_Cancer_Results_From_TROG_0202
[11]https://www.astro.org/news-and-publications/news-and-media-center/news-releases/2020/Astro-responds-to-CMS-Radiation-Oncology-Model-IMP
[12]https://www.astro.org/ASTRO/media/ASTRO/Patient%20Care%20and%20Research/PDFs/ROILS-in-Review_FistFiveYearsReport.pdf
[13] https://www.astro.org/Patient-Care-and-Research/Patient-Safety/RO-ILS/Case-Study-02
[14] https://www.astro.org/Patient-Care-and-Research/Patient-Safety/RO-ILS/Case-Study-02
[15]https://www.astro.org/ASTRO/media/ASTRO/Patient%20Care%20and%20Research/PDFs/ROILS-in-Review_FistFiveYearsReport.pdf
[16] https://aapm.onlinelibrary.wiley.com/doi/10.1002/mp.13526
[17]https://www.gehealthcare.com/article/interoperability-in-healthcare-how-medical-device-integration-is-helping-tear-down-those-walls