“Automated Breast Ultrasound Provides Comparable Diagnostic Performance in Opportunistic Screening and Diagnostic Assessment” study demonstrates the power of ABUS in breast cancer detection
Breast cancer: A growing public health problem
Breast cancer is the most commonly diagnosed cancer in the world, accounting for 1 in 8 cancer diagnoses.[1] A growing concern for women all over the globe, its prevalence continues to rise in many parts of the world, including countries in Asia. Nearly half of the 2.3 million breast cancers diagnosed worldwide in 2020 were in Asia, with many considered late-stage cancers.[1] Dense breasts, a risk factor for developing breast cancers, are more likely to present in Asian women compared to Caucasian women.[2] A majority of Malaysian women (59%) participating in a study had dense breasts.[2]
Addressing barriers to care
Many countries in Asia do not offer breast cancer mammography screening programs. Studies have cited a variety of potential barriers to mammography screening, including:
-
A lack of awareness of breast cancer and mammography screening, low health literacy/education
-
Personal beliefs, fear, religion, lack of support from loved ones
-
Sociodemographic factors, and financial constraints.[3]
While mammography is proven to help detect these cancers early, its sensitivity decreases in women with dense breasts, encouraging the use of alternative screening technology. Automated breast ultrasound (ABUS) is specifically designed to supplement mammography, detecting cancers in dense breast tissue that may not appear in a mammography.[4],[5]
To determine the impact of ABUS screening technology with digital breast tomosynthesis (DBT), a team led by Professor Dr. Kartini Rahmat conducted the first Association of Southeast Asian Nations (ASEAN) study of ABUS designed to assess the performance of the Invenia™ ABUS as an adjunct to DBT. This study evaluated 1089 women who underwent opportunistic screening with DBT between December 2019 and March 2022 for screening or diagnostic purposes. The women were offered additional ABUS examination in the same setting.
The positive impact of adjunctive ABUS in breast cancer morbidity and mortality
The results from this study showcased this technology as a transformative solution for developing countries with limited radiologists, and limited access to mammography. ABUS is useful as an adjunct to DBT in the opportunistic screening and diagnostic setting:
-
Without ABUS, potentially nine cancers would have been missed. These were detected by ABUS alone, with 77.8% of these being clinically relevant invasive cancers.
-
ABUS proved equally useful in non-dense and dense breasts because of the additional cancer detected. Of the 135 malignant lesions detected:
-
75.8% (106/135) of malignant lesions were detected by ABUS + DBT, 6.7% (9/135) using ABUS alone. 14.1% (19/135) using DBT alone while 52.6% of those were ductal carcinoma in situ (DCIS).
-
85.9% (116/135) were detected on the coronal view of ABUS.
-
-
The biopsy rate with the addition of ABUS to DBT in the screening population was 23.4%.
“Effective screening methods play a crucial role in addressing breast cancer, one of the leading causes of death worldwide in women,” said Professor Kartini Rahmat, Department of Biomedical Imaging, Universiti Malaya Research Imaging Centre, Universiti Malaya, Malaysia. “Our study underscores the fundamental role of ABUS as a complementary tool to mammography/DBT, and its ability to enhance cancer detection in dense and non-dense breasts and provide an additional layer of screening to prevent missed diagnoses.”
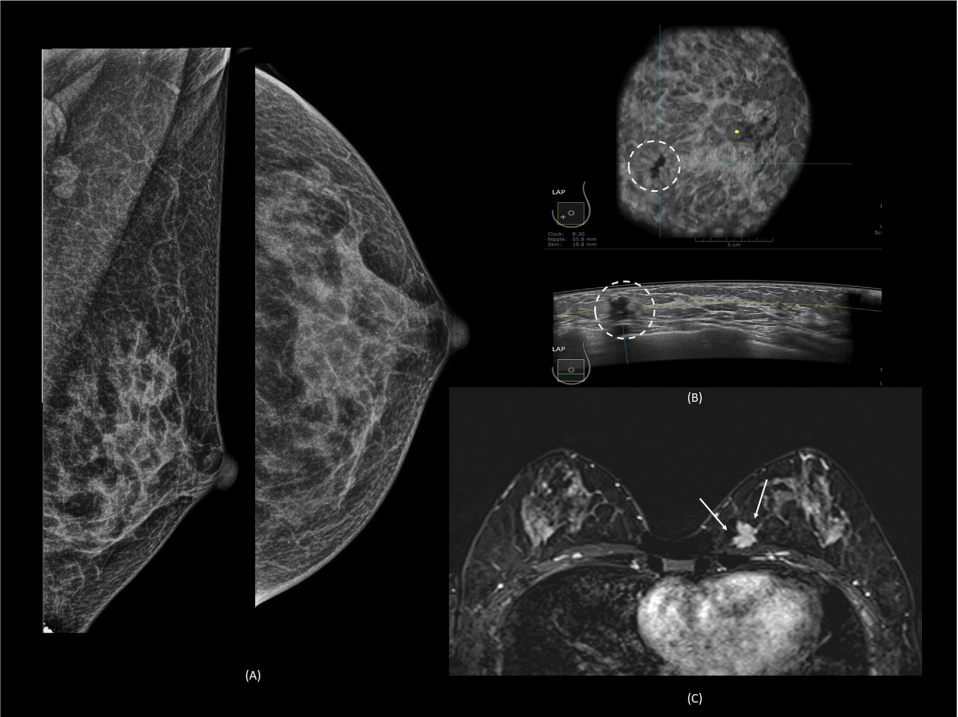
Forty-two-year-old woman with incidental finding of an enhancing left breast mass on computed tomography. The mammogram was normal (A). On automated breast ultrasound (ABUS) , there is a lobulated hypoechoic lesion with retraction sign on the coronal view and lobulated with spiculated margins on the axial view (dashed circle) (B). Magnetic resonance imaging revealed a heterogenous enhancing irregular mass with spiculations at the lower inner quadrant of the left breast (arrows) (C). This was histologically proven to be grade 2 invasive carcinoma.
ABUS is designed for advanced patient care, and has several features to improve comfort including multiple compression level options, a Reverse Curve™ transducer, designed to conform to a woman’s anatomy, and customizable protocols to ensure smooth and efficient scanning procedure. In comparison to other breast imaging technologies, ABUS is an accessible and affordable technology, and doesn't use any iodinated contrast agent or ionizing radiation. Supplemental screening with Invenia™ ABUS 2.0 transforms breast care from reactive to proactive, uncomfortable to comfortable, offering personalized breast care for early detection and confident diagnoses. A patient experience study showed that 100% of women would recommend an ABUS exam to their best friend.[6] Learn about more about The Power of ABUS and the Invenia ABUS.
[1] Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, Vignat J, Gralow JR, Cardoso F, Siesling S, Soerjomataram I. Current and future burden of breast cancer: Global statistics for 2020 and 2040. Breast. 2022 Dec;66:15-23. doi: 10.1016/j.breast.2022.08.010. Epub 2022 Sep 2. PMID: 36084384; PMCID: PMC9465273.
[2] Kartini Rahmat, Nazimah Ab Mumina, Wei Lin Nga , Nur Aishah Mohd Taibc , Wai Yee Chand , Marlina Tanty Ramli Hamid. Automated Breast Ultrasound Provides Comparable Diagnostic Performance in Opportunistic Screening and Diagnostic Assessment. Ultrasound in Medicine & Biology. 2023. https://doi.org/10.1016/j.ultrasmedbio.2023.09.011
[3] Lim YX, Lim ZL, Ho PJ, Li J. Breast Cancer in Asia: Incidence, Mortality, Early Detection, Mammography Programs, and Risk-Based Screening Initiatives. Cancers. 2022; 14(17):4218. https://doi.org/10.3390/cancers14174218
[4] Tagliafico, Massimo Calabrese et al, Journal of Clinical Oncology 2016 34:16, 1882-1888.
[5] Pisano et al. NEJM 2005; 353: 1773.
[6] Shah et.al. Journal of Diagnostic Medical Sonography DOI: 10.1177/8756479313476920 2013.