Polyethylene glycol (PEG) is a synthetic polyether compound used in various consumer and medical products—from body creams and cosmetics to the mRNA COVID-19 vaccines. PEG is nontoxic and inert; however, it still carries the potential to trigger hypersensitivity reactions. Incidentally, the rate of these reactions has increased in recent years, accelerating with the start of the COVID-19 vaccination program.1
The American Society of Echocardiography (ASE) released a statement addressing the rising rate of PEG hypersensitivity reactions, noting that while these reactions can occur, they remain rare. Overall, UEAs have an extremely low risk-to-benefit ratio—ASE stated—therefore, they should be used in situations where they have shown to be effective.
That said, ASE still provided recommendations and specific steps echo labs should take to manage the risk of hypersensitivity in their labs, including:
- Counseling patients that the frequency of severe reactions to UEAs is rare: 1 in 10,000.
- Training sonographers, nurses, and physicians who administer UEAs to recognize the symptoms of PEG hypersensitivity reactions.
- Screening patients for hypersensitivity to agents that contain PEG.
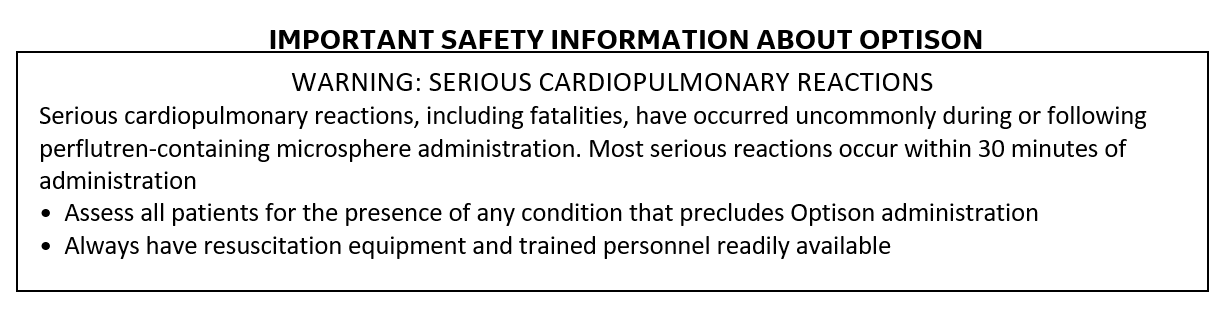
- Keeping cardiopulmonary resuscitation equipment readily available for use by trained personnel.3
This article—a featured piece in GE Healthcare’s series on PEG—will cover several of the American Society of Echocardiography’s actionable recommendations on PEG hypersensitivity risk management.
1. Screen patients for possible PEG hypersensitivity
Effective screening protocols can help echo labs determine whether patients have known or suspected PEG hypersensitivity so they can avoid the use of UEAs containing PEG. Screening processes would include:
- Asking patients about known allergies, including any drugs they are allergic to. Inquire about a history of reactions to UEAs or if they have a known PEG allergy. A history of adverse reactions to medical products containing PEG, such as MiraLax, can also be helpful information.
- Asking patients about their vaccination status. Data suggests a modest hypersensitivity cross-reactivity between COVID-19 vaccines and UEAs.5 Ask whether the patient is vaccinated and, if so, which vaccine they received. If a patient received either the Pfizer or Moderna vaccine, which contains PEG, ask if they had any adverse reaction to the vaccine or boosters.4
2. Recognize and manage PEG hypersensitivity reactions
Understanding the signs and symptoms of hypersensitivity reactions is critical for echo labs, since it may help staff identify these reactions early and act accordingly.
The largest study on PEG reactions and UEAs to date was published as a letter to the editor in the Journal of American Society of Echocardiography in February 2022. It reported on ten adverse reactions to PEG-containing UEAs, which occurred across three echo centers at the University of Pennsylvania Health System and Medical University of South Carolina between January 2019 and July 2021.
These adverse events included:
- Shortness of breath
- Tongue and throat swelling
- Abdominal and back pain
- Hemodynamic instability
- Arrhythmias
- Hypoxia6
3. Respond effectively to adverse UEA reactions
In addition to training staff on recognizing reactions, labs should have protocols, medications, and equipment in place and on hand to help manage adverse reactions, should they occur. For example, contact information for the cardiopulmonary arrest response team should be clearly posted, and a code cart must be available anytime the lab administers a UEA.4
Sonographers should immediately inform the lab’s attending physician if they suspect a patient is having an adverse reaction.4 If a severe reaction occurs, staff should immediately discontinue the UEA injection (if not completed) and administer an H1 receptor blocker. If the reaction is severe or widely disseminated, epinephrine should be administered.4
Labs should also keep emergency equipment on hand, in compliance with hospital protocols.
Avoid hypersensitivity reactions with a PEG-free UEA
With PEG hypersensitivity on the rise, echo labs should consider stocking a UEA that does not contain PEG. Three of the four FDA-approved UEAs contain PEG—but Optison™ (Perflutren Protein-Type A Microspheres Injectable Suspension, USP) does not. Please scroll to the bottom of this blog to see Important Safety Information about Optison.
As a PEG-free option for enhancing ultrasound image quality, Optison can be used in patients with a history of adverse reactions to PEG. In a recent GE Healthcare-sponsored webinar, Dr. Richard Weiss, Director of Echocardiography at Penn Presbyterian Medical Center, and Rodney Jefferson, RDCS, RCS, echocardiographer at Hunterdon Medical Center in New Jersey, recommended using Optison—highlighting that they found this UEA especially helpful in cases where a patient had multiple allergies.4 Optison also has a well-established safety profile for patients aged 18 and up7-9, helping provide peace of mind for both patients and providers.
In addition, Optison:
- Remains stable at room temperature for up to 24 hours.
- Does not require a machine for preparing to administer.
- Can go from suspension to administration in less than 1 minute. 9
- Helps save staff time, as they can bypass PEG hypersensitivity screenings. 9
Learn more about Optison and how it can help enhance ultrasound image quality in your lab—without PEG.
REFERENCES
- Garvey LH, et al. Anaphylaxis to the first COVID-19 vaccine: is polyethylene glycol (PEG) the culprit? Br J Anaesth. 2021;126(3):e106-e132.
- https://www.acr.org/Advocacy-and-Economics/Advocacy-News/Advocacy-News-Issues/In-the-April-24-2021-Issue/FDA-Warns-Against-Some-Ultrasound-Contrast-Agents. Accessed May 26, 2022.
- Lindner JR, et al. Expert consensus statement from the American Society of Echocardiography on hypersensitivity reactions to ultrasound enhancing agents in patients with allergy to polyethylene glycol. J Am Soc Echocardiogr. 2021;34(7):707-708.
- Jefferson, RT and Weiss, RL. 2022. What Echo Labs Need to Know about PEG [webinar]. GE Healthcare.
- Desai AK, Hodovan J, Belcik JT, Lindner JR. Hypersensitivity Cross-Reactivity for Ultrasound-Enhancing Agents and COVID-19 Vaccines. J Am Soc Echocardiogr. 2022;35(5):523-525. doi:10.1016/j.echo.2022.02.006
- Soni M, et al. Ultrasound-enhancing agents and associated adverse reactions: a potential connection to the COVID-19 vaccines? J Am Soc Echocardiogr. 2022;35(2):241-242
- Wei K, Shah S, Jaber WA, DeMaria A. An observational study of the occurrence of serious adverse reactions among patients who receive optison in routine medical practice. J Am Soc Echocardiogr. 2014;27:1006-1010.
- Exuzides A, Main ML, Colby C, Grayburn PA, Feinstein SB, Goldman JH. A retrospective comparison of mortality in critically ill hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent. JACC Cardiovasc Imaging. 2010;3:578-585.
- Main ML, Grayburn PA, Lang RM, et al. Effect of Optison on pulmonary artery systolic pressure and pulmonary vascular resistance. Am J Cardiol. 2013;112:1657-1661.
- Optison [prescribing information]. Marlborough, MA: GE Healthcare. 2021.
INDICATIONS AND USAGE: OPTISON is indicated for use in patients with suboptimal echocardiograms to opacify the left ventricle and to improve the delineation of the left ventricular endocardial borders.
CONTRAINDICATION: Do not administer OPTISON to patients with known or suspected hypersensitivity to perflutren or albumin.
ADVERSE EVENTS: The most frequently reported adverse reactions in clinical trials were headache, nausea and/or vomiting, warm sensation or flushing and dizziness. Cardiac arrests and other serious but nonfatal adverse reactions were uncommonly reported in post-approval use. Reports also identified neurologic reactions (loss of consciousness or convulsions) as well as anaphylactoid reactions.
Please see Full Prescribing Information for Optison here.
JB06997US