Positron Emission Tomography (PET), a functional imaging modality, is an indispensable medical imaging technique.[1] however with innovations on-going, it continues to push the limits of PET detector technology to maximize sensitivity and are propelling molecular imaging into the future. Following its combination with computed tomography (CT), PET/CT imaging has grown in utilization across specialties—and most notably in oncology imaging. For the benefit of these and other patients, PET sensitivity is a key component of the imaging data analyzed to determine their care. Using state-of-the-art detector technology in conjunction with the imaging agent 18F-fluorodeoxyglucose (FDG), PET imaging characterizes oncologic tumors based on biochemical changes at the molecular level.
Increases in demand for PET/CT imaging and innovations in PET technology—fueled by the increase in the prevalence of diseases such as cancer that it can detect—have boosted the growth of the global PET/CT scanner device market. The COVID-19 pandemic also impacted demand for PET/CT imaging because of its ability to help monitor infection at the molecular level. In a report published by Allied Market Research, the global PET/CT scanner device market generated $1.87 billion in 2020 and is expected to reach $3.20 billion by 2030.[2],[3]
Molecular imaging (MI), specifically the diagnostic power of PET imaging, plays a key role in enabling precision medicine and benefits from the evolution of improvements in the system’s sensitivity to continually enhance image quality and to help create more flexible options for lowering doses or shortening patient scan times.
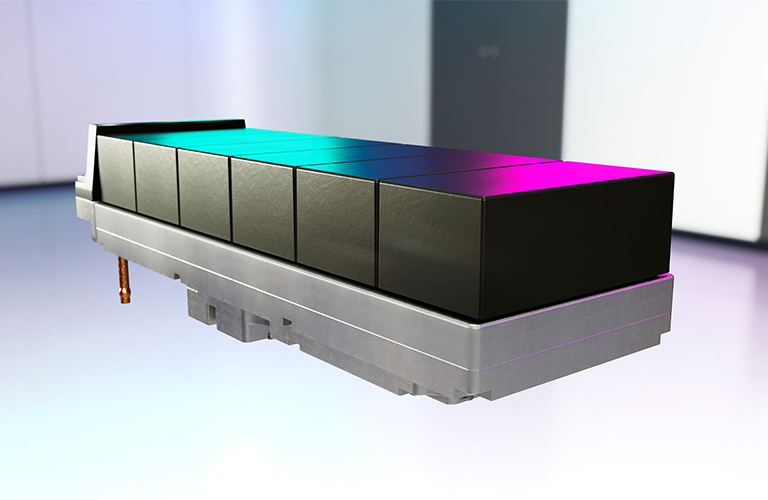
“In molecular imaging, we’re innovating PET with sophisticated digital detector and crystal technology to augment NEMA sensitivity levels and generate the maximum amount of raw imaging data possible,” said Erez Levy, Executive Director and General Manager for Molecular Imaging at GE Healthcare. “As we move into a future where artificial intelligence (AI) and deep learning technologies enable new types of image processing and clinical decision support, having those data points is crucial, as they give clinicians more flexibility in imaging for their patients without any sacrifice to image quality.”
Innovations in PET detector technology for improved scanner sensitivity
Improvements to the quality of PET images are made by increasing the sensitivity and spatial resolution of the image, which requires an array of detectors that can capture the largest possible fraction of the photons emitted by the target object at the highest possible rate and with the best possible spatial accuracy. In addition, PET detectors should possess the highest possible energy resolution to reduce the effects of scattered radiation.[4]
PET detectors capture and measure the two annihilation photons, or counts, that are produced back-to-back after positron emission from the tracer molecule, which is chosen to highlight a specific function in the body on a biochemistry level. The photons released are detected by coincidence imaging as they strike scintillation crystals made of either bismuth germanate (BGO), lutetium oxyorthosilicate (LSO), or gadolinium silicate (GSO).[5] The sensitivity of a PET scanner is determined by calculating the number of 511-keV photon pairs per unit of time detected by the device for each unit of activity present in a source. This calculation is usually expressed in counts per second per microcurie or megabecquerel (cps/microCi or cps/kBq).[6]
Innovations in PET crystal utilization and the introduction of digital detectors offer new directions and possibilities that expand the clinical utilization of PET. These include scanners with:
- Higher geometric coverage of the body
- More sensitive and compact silicon photomultiplier light sensors
- Detectors able to handle ultra-high count rate flux
Moreover, these improved detector electronics will combine with computational methods including deep learning and AI to better estimate the location, time, and energy of an interaction in the detector.
The importance of NEMA sensitivity
The molecular imaging industry uses the universally accepted guidelines on PET sensitivity from the National Electrical Manufacturers Association (NEMA) as a uniform and consistent method for measuring and reporting the performance parameters of PET scanners. PET scanners are designed to meet certain NEMA performance standards, and each PET scanner is routinely evaluated throughout its clinical use to verify Image Quality performance. Variations in scanner designs from manufacturers across the industry can cause PET scanners to have different sensitivities to scattered radiation, but ultimately, every scanner must meet the NEMA sensitivity capabilities as specified by its manufacturer. Manufacturers such as GE Healthcare consistently strive to maximize the NEMA sensitivity on their systems.
As the industry standard, NEMA sensitivity has been used in many published studies as a variable in evaluating the performance of PET detectors (either alone or compared to other types of detectors) and in studies analyzing different diseases using PET/CT imaging.
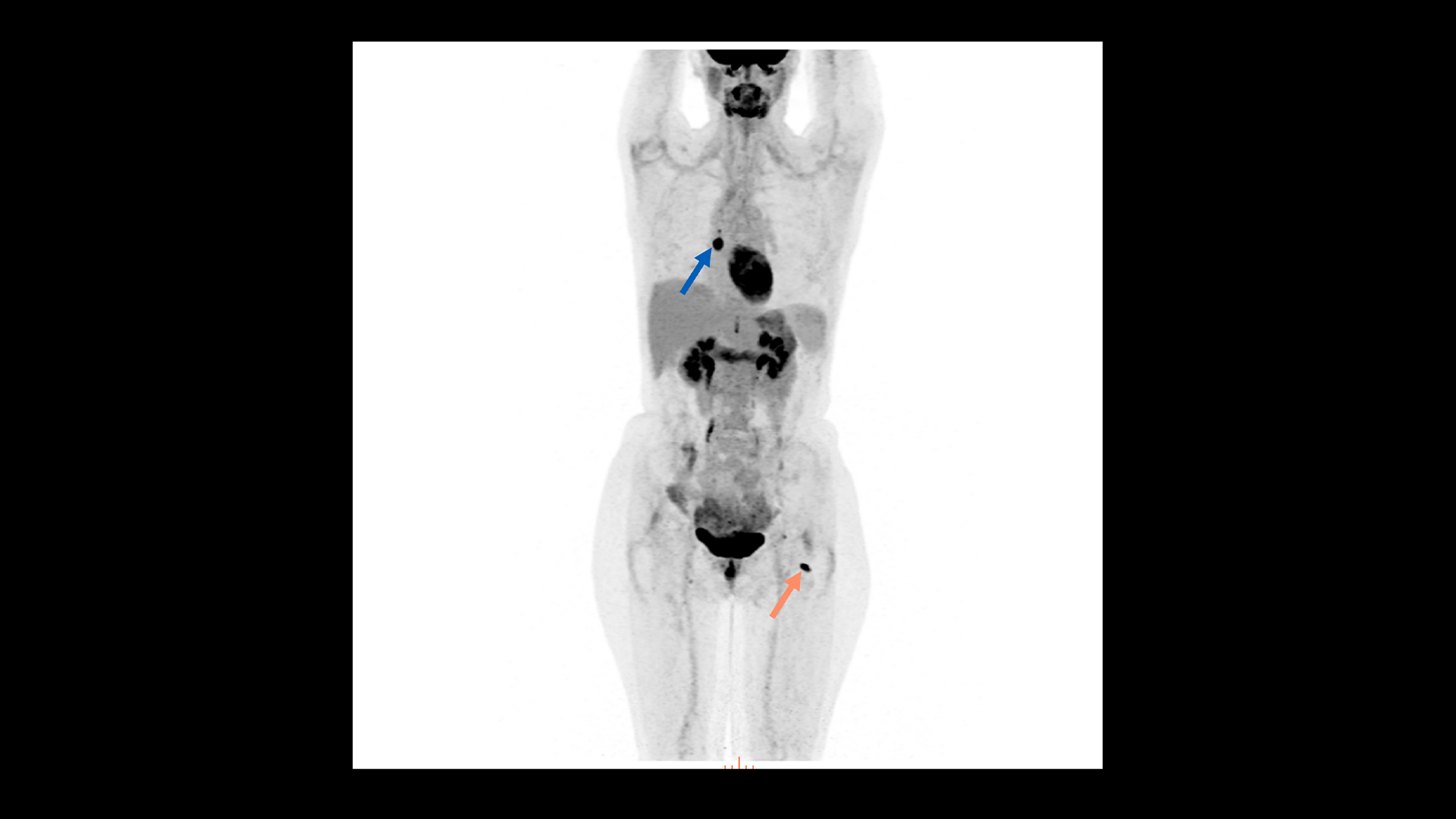
Many of these studies conclude that higher sensitivity levels can benefit image quality and can offer increased flexibility in adjusting acquisition time or radiation dose without limiting image quality. System performance and clinical imaging were compared between one system and other commercially available PET/CT and PET/MR systems, as well as between different reconstruction algorithms. In the evaluation, spatial resolution, sensitivity, noise-equivalent counting rate, scatter fraction, counting rate accuracy, and image quality were characterized using NEMA performance standards. The study concluded that a higher sensitivity allows for better signal-to-noise (SNR) ratio for a given acquisition time and the same SNR for shortened acquisitions or reduced dose to the patient.[7]
Maintaining image quality with shortened acquisition times or reduced patient dose is often evaluated in clinical studies. From the patient’s perspective, PET imaging is commonly associated with these two areas of concern: exposure to radiation, as many patients will have repeated studies over time, and the discomfort of lying as still as possible for 10–20 minutes (knowing that even small movements might blur the images and reduce the accuracy of diagnostic interpretation). However, reducing dose or scan time typically requires a sacrifice in image quality because a reduced number of annihilation events are collected.[8] Therefore, to enable shorter scan times or lower dose, system performance has to be improved. This can be achieved by increasing the NEMA sensitivity of the scanner and/or by improving the timing resolution,[9], which is why PET detector performance and sensitivity are so often the topics of clinical studies.
Another study comparing PET detector performance in the standard uptake values (SUV) of liver lesions suggests that higher sensitivity levels and improved reconstruction algorithms will lead to increased detection of pathology, such as earlier detection of small lesions. The study showed improved lesion visibility and higher SUV values on one type of PET/CT system and concluded that the greater SUV is likely explained by the greater sensitivity and different reconstruction algorithm that was used.[10]
Enabling personalized care with PET/CT and improving access to essential imaging technologies
As a mature industry, molecular imaging’s next frontier is personal; this field holds the potential to deliver on the promise of precision medicine and personalized care. As PET technology evolves, the ability for clinicians to personalize imaging based on clinical needs for higher image quality or to reduce patient dose or scan times becomes even more accessible. In addition, the development of novel radioisotopes and targeted therapeutic pairings, coupled with superior image quality, make advanced diagnoses and targeted treatments possible. Advances in radiopharmaceutical development and molecular imaging technology continue to reinforce molecular medicine’s key role in patient management.
With upgrades in scanner hardware, software, or both, healthcare providers can access innovations in PET technology, can extend the life of their existing imaging equipment, and expand their clinical capabilities without needing to purchase new systems. Newer PET/CT system platforms can improve detector technology using larger detectors and enhance image quality using powerful deep-learning and AI-based software.
Medical imaging technology continues to be one of the most essential diagnostic tools available. GE Healthcare is committed to advancing both imaging hardware and software power with high-performance solutions for various imaging modalities—including molecular imaging—allowing these systems to rapidly process massive amounts of image data, streamline workflows, and improve the patient care experience.
Learn more about GE Healthcare’s latest PET/CT, Omni Legend to help advance your patient outcome.
DISCLAIMERS
Not all products or features are available in all geographies. Check with your local GE Healthcare representative for availability in your country.
Omni Legend and Precision DL are CE marked. Omni Legend is 510k-cleared by the US FDA. Precision DL is 510k-pending with the US FDA. Not available for sale in the United States. Clinical images shown was processed with Precision DL and obtained from an investigational device, limited by U.S. law to investigational use.
REFERENCES
[1] https://jnm.snmjournals.org/content/59/1/3
[2] https://www.alliedmarketresearch.com/pet-ct-scanner-device-market
[3] https://www.itnonline.com/content/global-pet-ct-scanner-device-market-hit-320-billion-2030
[4] Peng BH, Levin CS. Recent developments in PET instrumentation. Curr. Pharm. Biotechnol. 2010;11(6):555–571. https://pubmed.ncbi.nlm.nih.gov/20497121/
[5] Jha AK, Mithun S, Puranik AD, Purandare NC, Shah S, Agrawal A, Rangarajan V. Performance characteristic evaluation of a bismuth germanate-based high-sensitivity 5-ring discovery image quality positron emission tomography/computed tomography system as per National Electrical Manufacturers Association NU 2-2012. World J Nucl Med. 2019 Dec 18;18(4):351-360.
[6] Vandenberghe, S., Moskal, P., & Karp, J. S. (2020). State of the art in total body PET. EJNMMI Physics, 7(1), 1-33. https://doi.org/10.1186/s40658-020-00290-2
[7] Hsu DFC, Ilan E, Peterson WT, Uribe J, Lubberink M, Levin CS. Studies of a Next-Generation Silicon-Photomultiplier-Based Time-of-Flight PET/CT System. J Nucl Med. 2017 Sep;58(9):1511-1518. doi: 10.2967/jnumed.117.189514. Epub 2017 Apr 27. PMID: 28450566.
[8] Berg, E., & Cherry, S. R. (2018). Innovations in instrumentation for positron emission tomography. Seminars in nuclear medicine, 48(4), 311. https://doi.org/10.1053/j.semnuclmed.2018.02.006
[9] Berg, E., & Cherry, S. R. (2018). Innovations in instrumentation for positron emission tomography. Seminars in nuclear medicine, 48(4), 311. https://doi.org/10.1053/j.semnuclmed.2018.02.006
[10] Oddstig, J., Leide Svegborn, S., Almquist, H. et al. Comparison of conventional and Si-photomultiplier-based PET systems for image quality and diagnostic performance. BMC Med Imaging 19, 81 (2019). https://doi.org/10.1186/s12880-019-0377-6. https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-019-0377-6