By Sarah Handzel, BSN, RN
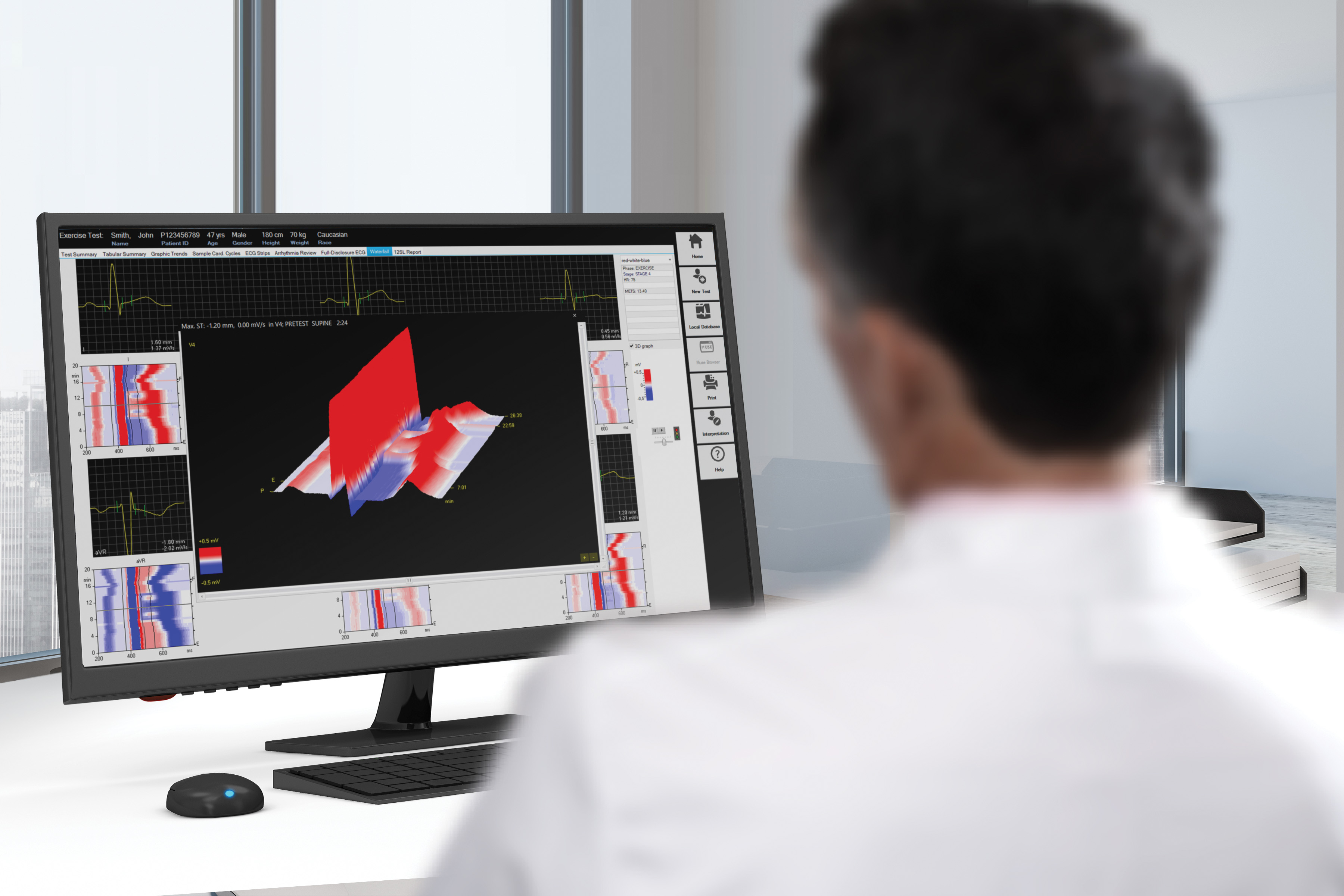
Cardiac stress testing is an important modality used in the diagnosis and management of patients with suspected coronary artery disease (CAD) and other cardiovascular abnormalities. Beyond diagnosis, stress tests may also reveal a patient's response to treatment and guide further therapeutic decisions. ECGs recorded during stress tests—whether functional or pharmacological—show essential data relating to arrhythmias, coronary artery blockages, valve problems, and other issues affecting the patient's cardiovascular health; these variables may then be used to help determine a patient's risk for cardiovascular events.
To be effective, a stress test must raise a patient's heart rate to a specific target range sufficient to dilate coronary arteries while increasing myocardial oxygen demand; generally, patients should be stimulated to about 85% of their age-related maximum heart rate. This target may be calculated by subtracting the patient's age from 220.1
Physicians should carefully review the indications and contraindications for the two types of cardiac stress testing: dynamic (or exercise) and pharmacologic. Although functional stress testing is generally considered ideal, some patients cannot tolerate exercise and must receive a specific medication to raise their heart rate without exertion.
Dynamic Stress Tests
Dynamic stress tests using a treadmill, bicycle, or other mechanical means help physicians identify problems like ischemia through stimulation of the sympathetic nervous system, which promotes coronary vasodilation and allows for greater perfusion of oxygen-rich blood to myocardial tissue.1 Exercise stress tests also allow for functional assessment by measuring oxygen consumption during exercise; test results indicate a patient's ability to perform work and other daily activities requiring exertion.2
Pharmacologic Stress Tests
In contrast to those suited for exercise cardiac stress tests, ideal candidates for pharma stress tests are those unable to perform exercise due to a variety of medical conditions, including:3
- Acute pulmonary embolism or inflammation of the peri- or myocardium
- Myocardial infarction within one week
- Poorly managed blood pressure with systolic readings greater than or equal to 200mmHg while resting
- Previous diagnosis of heart failure that is not well managed
- Severe pulmonary hypertension
- Unstable angina
Currently, FDA-cleared vasodilators include adenosine, dipyridamole, and regadenoson. Contraindications are specific to each medication, and providers should review safety information for each before selecting which drug to use.4 Today, most providers prefer regadenoson as it selectively targets A2A receptors and generally causes fewer side effects.3 However, dobutamine may be used in patients with severe respiratory diseases, including chronic obstructive pulmonary disease or asthma.3
Determining Which Exercise Modality to Use
To produce pertinent results, dynamic exercise testing must induce myocardial ischemia via increased demand for oxygen.5 Generally, isotonic exercises, such as upright bicycling or running on a treadmill, increases both blood pressure and heart rate in response to greater exercise intensity. However, venous return is typically more markedly increased when the patient is in the recumbent position.5
The ultimate goal of isotonic exercise is to evaluate cardiac output in response to increased oxygen demand.5 The exercise session should cease when target heart rate is reached, or when the patient cannot tolerate exercise any longer. Treadmill stress tests should provide information about arrhythmias and ST segment changes with both ECG and ultrasound; supine bicycle exercise tests provide the same information, although stress-induced cardiac changes may be more likely to resolve before capture on various types of recordings.5 However, supine bicycle testing does allow images to be captured during testing, resulting in more data collected over a longer period of time.5
Regardless of the type of dynamic exercise completed, the patient's metabolic equivalents (METS) may be used to predict certain cardiovascular problems. For example, those unable to achieve five or more METS are generally at higher risk for coronary artery disease events.6 In contrast, those achieving 10 METS or more have a much lower risk of coronary artery disease events.6
From the exercise test results, physicians should be able to evaluate data for information regarding coronary artery disease, cardiac risk prediction, and overall functional results. Dynamic testing allows for the collection of such data, whereas pharmacological testing generally cannot provide enough information for the comprehensive assessment of all elements.
Limitations to Pharmacologic Stress Testing
Unfortunately, pharmacologic stress testing generally cannot yield results as comprehensive and accurate as dynamic stress testing. Additionally, patients with high CAD pretest probability are more likely to receive false-negative results; therefore, intermediate CAD probability patients are most likely to benefit from this procedure. Interfering factors include caffeine, methylxanthines, and beta-blockers, depending on the vasodilator used.3
METS measurements during pure pharmacologic testing are also generally much lower compared to dynamic exercise testing, negating the possible benefits of this strong predictive value. Other measurements, including heart rate recovery, are also affected by the pharmacological test's inability to stimulate heart rate to its target, resulting in potentially inaccurate interpretation of test results.
Exercise stress tests are the most preferred modality for obtaining ECG information about a heart performing work. Information gained from tests based on physical exertion reveal more about about each patient's functional capacity, exercise tolerance, and factors resulting in symptoms.3 Sudden cardiac death risk is significantly elevated with a high resting heart rate (>75 b.p.m.), a limited heart rate increase during exercise (<89 b.p.m.), or a sluggish heart rate recovery (<25 b.p.m.). Thus, greater total physical activity each week can increase sympathetic activity and lead to a well-balanced autonomic tone.7
Generally, cardiac stress testing of either modality is considered safe, but patients may still suffer from unexpected side effects, especially during pharmacologic stress testing, depending on the agent used. However, given the potential diagnostic benefits of stress tests, this relatively simple and inexpensive procedure will continue to aid providers and patients alike.
Resources:
- Vilcant V, Zeltser R. Treadmill stress testing. StatPearls Publishing. 2022. https://www.ncbi.nlm.nih.gov/books/NBK499903/.
- Piepoli MF, Spoletini I, Rosano G. Monitoring functional capacity in heart failure. European Heart Journal Supplements. 2019;21 (M):M9-M12. https://doi.org/10.1093/eurheartj/suz216
- Lak HM, Ranka S, Goyal A. Pharmacologic stress testing. StatPearls Publishing. 2022. https://www.ncbi.nlm.nih.gov/books/NBK555963/
- Irving JB, Bruce RA, DeRouen TA. Variations in and significance of systolic pressure during maximal exercise (treadmill) testing. The American Journal of Cardiology. 1977; 39(6):841-848. https://doi.org/10.1016/S0002-9149(77)80037-4
- Suzuki K, Hirano Y, Yamada H, et al. Practical guidance for the implementation of stress echocardiography. J Echocardiogr. 2018;16(3):105-129. https://link.springer.com/article/10.1007/s12574-018-0382-8#Sec2
- Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain. Journal of the American College of Cardiology. 2021;78(22):e187-e285. https://www.jacc.org/doi/10.1016/j.jacc.2021.07.053
- Wellens, H. J. J., P. J. Schwartz, F. W. Lindemans, et al. Risk Stratification for Sudden Cardiac Death: Current Status and Challenges for the Future. European Heart Journal. 2014; 35 (25): 1642–51. https://doi.org/10.1093/eurheartj/ehu176.
Sarah Handzel, BSN, RN, has been writing professionally since 2016 after spending over nine years in clinical practice in various specialties.
The opinions, beliefs and viewpoints expressed in this article are solely those of the author and do not necessarily reflect the opinions, beliefs and viewpoints of GE Healthcare. The author is a paid consultant for GE Healthcare and was compensated for creation of this article.