Prostate cancer has long been one of the most prevalent malignancies affecting men worldwide. However, in recent years, significant progress has been made in the diagnosis and treatment options for prostate cancer patients. Advanced imaging diagnostics has led to an increased understanding of the disease and a paradigm shift toward improved accuracy in diagnosis and treatment.
To promote the latest in clinical collaboration across prostate cancer care, GE HealthCare brought together leading experts in the field of oncology and urology to discuss the latest advancements across the prostate cancer pathway. The speakers examined clinical applications of the most recent advances in imaging and treatments for prostate cancer, shedding light on the significant progress that continues to be made across the care pathway and the increasing precision and targeting enabled by advanced technologies, improving outcomes for prostate cancer patients, as well as what may be on the horizon in terms of predictive care.
Advancing accuracy in prostate cancer diagnosis with high-quality imaging
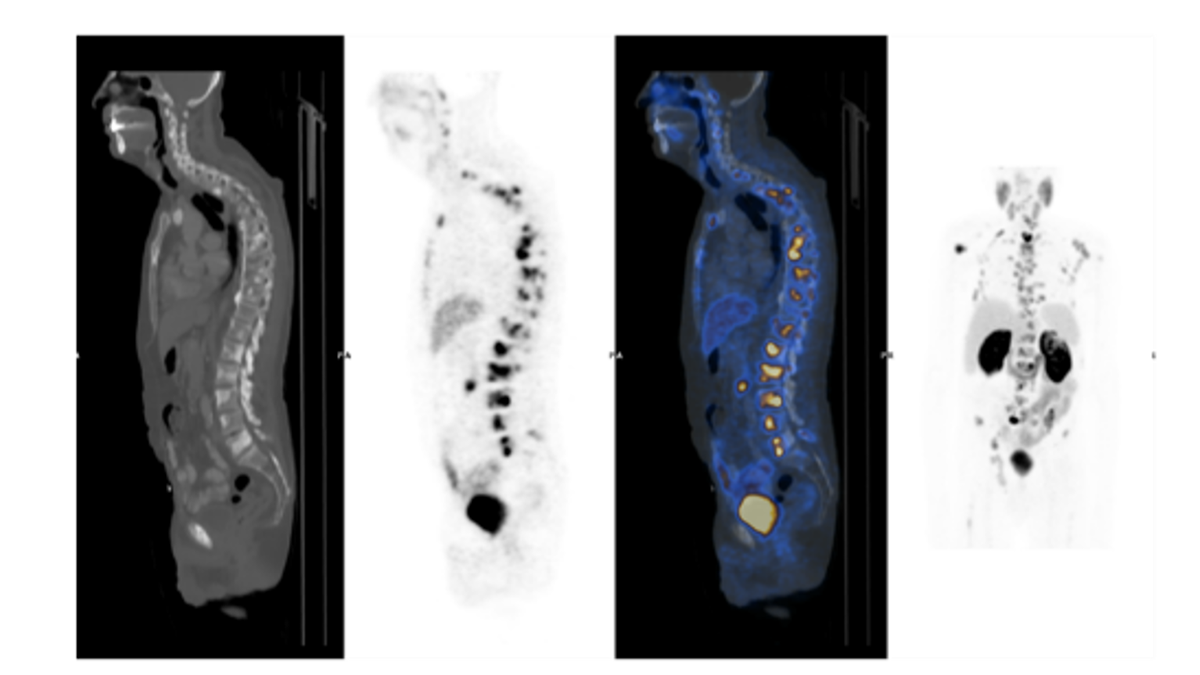
The panelists discussed the crucial role of accurate diagnosis in prostate cancer management. Advances in diagnostics and imaging techniques using magnetic resonance imaging (MRI) and positron emission tomography (PET) have significantly impacted disease detection and diagnosis compared to earlier standards of care in diagnosing and treating prostate cancer patients.
“Years ago, we were not able to create a visualization of prostate cancer for diagnosis,” explained Dr. Harun Fajkovic, a urologist with the Medical University of Vienna, Austria. “The introduction of the Prostate-specific antigen (PSA) biomarker was helpful, but it’s not a tumor marker. It’s an organ-specific marker, so patients with other conditions could also express higher levels of PSA. As a urologist performing brachytherapy treatments at that time, we were relying on ultrasound, but we had no ability to localize the lesion. When we began imaging the prostate with MRI and now with PET, we learned a lot. Today, if advanced imaging can show me a 5mm lesion in a transitional zone, I can effectively position the most appropriate brachytherapy treatment while minimizing potential adverse effects for my patient.”
According to Dr. Fajkovic, improved accuracy in prostate cancer diagnosis with imaging technologies such as MRI and PET has now led to improved oncologic control of tumors in the prostate. But he stipulated that this often comes at the expense of the patient’s quality of life, resulting in high incidences of incontinence and impotence as adverse effects of treatment, which are not optimal for his patients. Because of the advances in imaging technology available for diagnosing and guiding treatments for prostate cancer, Dr. Fajkovic has improved outcomes for his patients, effectively diagnosing and treating their disease while reducing the incidence of adverse effects from treatment. Currently, multiparametric MRI scanning (mpMRI) is viewed as the most precise imaging method for the detection of suspected prostate cancer.[1]
“From my own observations,” explained Dr. Hanna Falinska, a radiologist with Affidea Radiology Services in Poland, “the use of MRI for prostate cancer diagnosis is rising. Specifically, using the multiparametric protocol in MRI allows for morphologic and functional assessment of the prostate gland. It is a highly reliable imaging method to exclude clinically significant prostate cancer. Its capabilities in terms of image quality are key for us as we assess patient care pathways.”
In light of the increasing use of MRI to diagnose and guide prostate cancer treatment to improve early diagnosis and treatment of prostate cancer, the American College of Radiology (ACR), AdMeTech Foundation, and European Society of Urogenital Radiology (ESUR) formed a joint effort to develop standards for the Prostate Imaging Reporting and Data System (PI-RADS®).[2] The effort standardized terminology and content with structured reporting and created a five-point scale to assess clinically significant prostate cancer presence and to reduce unnecessary biopsies and treatment for benign and subclinical diseases.[3]
“I use these tools every day to assess categories for patient care pathways,” explained Dr. Falinska. “now clinicians and industry are working together to strengthen prevention with early detection of prostate cancer. In support of these efforts, current recommendations for prostate cancer detection include PSA antigen testing for men in combination with additional resonance imaging scanning as a follow-up test.”
Innovating treatment strategies with biomarkers and precision medicine
In recent years, advanced imaging technology, biomarkers, and innovative treatment strategies transformed the management of prostate cancer, allowing clinicians to identify subtypes of prostate cancer, tailor treatment plans, maximize efficacy, and minimize potential adverse effects for patients. Survival rates for prostate cancer are improving. In the US, the 5-year relative survival rate for prostate cancer is 97 percent.B[4] According to data from the Eurocare project, the 5-year relative survival rate for prostate cancers is 83 percent.[5] Variations in prostate cancer survival rates can be impacted by several factors, including the stage and grade of the prostate cancer, a person's age and general health, and how well a treatment plan works.
The panel discussed the effectiveness of standard treatment strategies for prostate cancer, including surgical prostatectomy, radiation therapies such as external beam radiation therapy and brachytherapy, and chemotherapy. They also discussed how treatments have evolved to now include hormone and biological therapies, high-intensity focused ultrasound, and promising therapies such as Theranostics.
As a breakthrough approach to treating prostate cancer, Theranostics integrates imaging diagnostics and targeted therapeutics for individualized management and treatment of disease. To date, Theranostics radiotherapy agents such as Lutetium-177 PSMA (LuPSMA) radionuclide therapy have been approved for use in metastatic prostate cancers, but many other agents are currently in discovery and trials, and more therapeutic agents are widely anticipated.
“Theranostics is helping improve prostate cancer management,” explained Dr. Guido de Lussanet de la Sabloniere, Radiologist at Erasmus MC in Rotterdam, Netherlands. “We select patients for this therapy if we believe the treatment will be successful for them, based on the information we have about their cancer. The importance of thoughtful patient selection and dosimetry cannot be underestimated as we continue to improve Theranostics treatment strategies for prostate cancer patients.”
Advancing precision medicine across the prostate cancer pathway
While advancements in prostate cancer treatments, especially newer therapies such as Theranostics, have shown promising results, the complexity of prostate cancer care has increased exponentially. Healthcare providers need to share diagnostic and pathology information as they select the most effective treatments for each patient, as well as monitor patients’ post-treatment data. Healthcare industry partners, such as GE HealthCare, recognize the impact that improving the coordination of prostate cancer care can have and the vital role they can play in improving patient outcomes.
From prostate cancer diagnosis to treatment, tools such as imaging data, artificial intelligence (AI), advanced clinical applications, biomarkers, and therapeutics are especially poised to help inform clinicians’ personalized approach to each patient’s care. Utilizing GE HealthCare’s newly introduced remote monitoring software for recovering patients offers clinicians the ability to communicate with each other through data streams on a system that’s stable and can aggregate patient data for analysis.
Dr. John Kelly, Urologist with the University College Hospital in London, England, is working with an evolving AI-based software concept to conduct high-performance remote patient monitoring for high-quality care.
“We’ve added biometric data to our analytics engine, which generates powerful insight when combined with EMR data, imaging data, and genomic streams,” Dr. Kelly explained. “We can improve outcomes today for prostate cancer patients by accurately predicting continence rates in 12 months post-treatment. In other scenarios, we are looking to reduce readmission rates based on remote monitoring data and combined with other patient information such as nutrition and physical activity.”
GE HealthCare is committed to working with leading clinicians to transform prostate cancer care through the development of advanced new technologies like these, driving precision medicine and collaborative clinical environments with the goal of improving healthcare outcomes for patients. The accuracy and early detection enhanced by medical imaging advancements as well as innovative treatments have catalyzed a transformative impact on prostate cancer management. By precisely characterizing tumors, clinicians can tailor personalized treatment plans based on the patient's unique disease profile. This tailored approach translates to improved outcomes, reduced treatment-related side effects, and enhanced patient quality of life.
Additionally, the power of medical imaging can extend beyond diagnosis to influence the monitoring and assessment of treatment response. Advanced imaging techniques enable real-time evaluation of treatment efficacy, empowering clinicians to make timely adjustments as necessary, further elevating the chances of successful patient outcomes.
RELATED CONTENT
View on-demand: Theranostics realities - navigating patient care complexity.
DISCLAIMER
Not all products or features are available in all geographies. Check with your local GE HealthCare representative for availability in your country.
REFERENCES
[1] Schlemmer HP, Krause BJ, Schütz V, Bonekamp D, Schwarzenböck SM, Hohenfellner M. Imaging of Prostate Cancer. Dtsch Arztebl Int. 2021 Oct 22;118(42):713-719. doi: 10.3238/arztebl.m2021.0309. PMID: 34427180; PMCID: PMC8767150.
[2] https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/PI-RADS
[3] https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/PI-RADS
[4] https://www.cancer.net/cancer-types/prostate-cancer/statistics#:~:text=The%205%2Dyear%20relative%20survival%20rate%20for%20prostate%20cancer%20in,vary%20based%20on%20several%20factors.
[5] https://publications.jrc.ec.europa.eu/repository/handle/JRC101382