The ECG has long been a mainstay of medical diagnosis, one that has had beneficial impacts across specialties. To get the most out of the technology, artifact-free readings are essential. There are various approaches to ECG signal filtering to remove noise and get a clean ECG signal, but clinicians must be aware of how these filters can affect the reading and only use them when other means have proven unsuccessful.
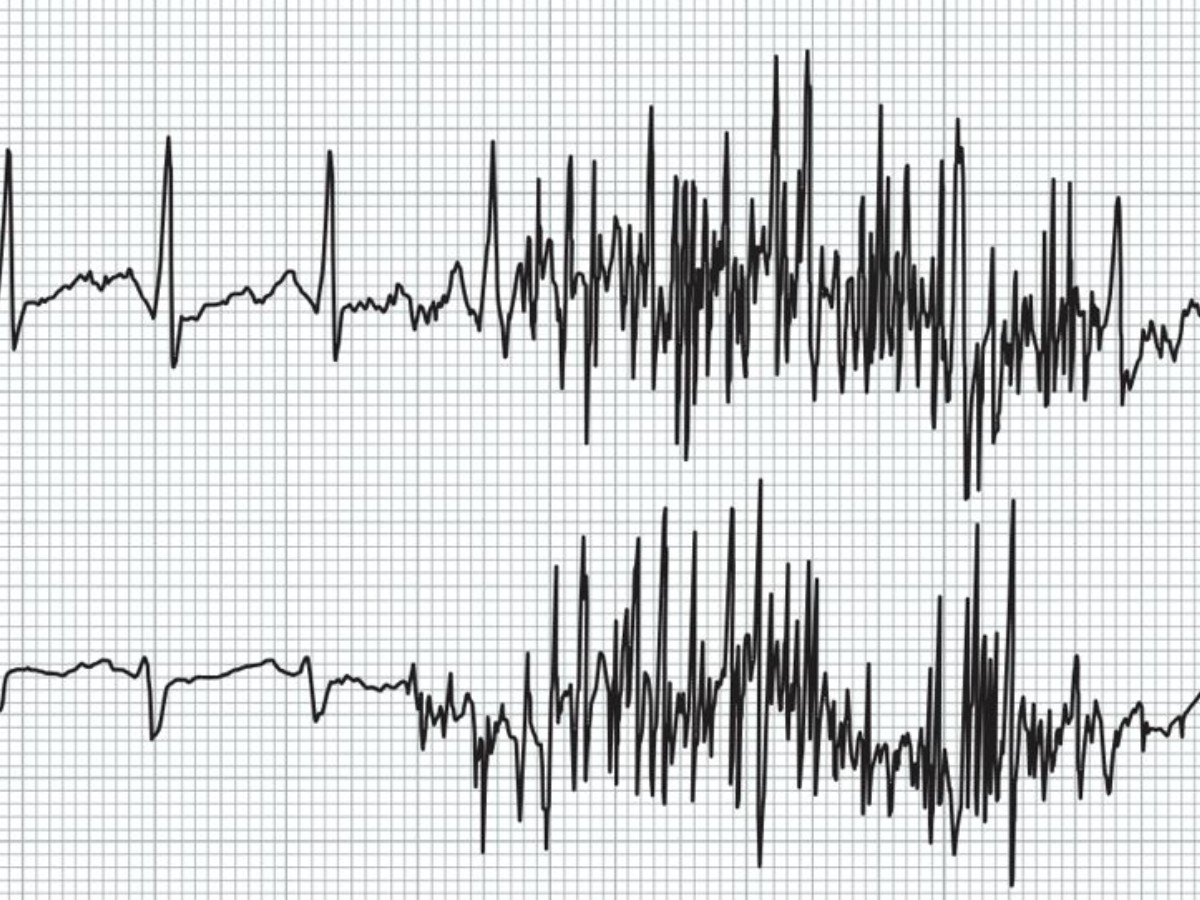
Contamination of an ECG signal comes from a variety of sources within and outside of patients' bodies. Electrical signals from other muscles besides the heart, as well as breathing, coughing, and other types of movement, can create artifacts. Noise can also come from poor electrical connections if the electrodes are not properly placed on the patient. Moreover, ECG leads are effective antennas that readily pick up sources of electrical noise from the immediate environment, including fluorescent lights, cell phones, or Bluetooth-enabled devices.
The Role of ECG Signal Filtering
All of these things can create a fuzzy ECG reading, much like snow on a television with a poor signal (prior to the advent of cable). Fortunately, there are several types of filters you can use to mitigate this interference. ECG frequencies typically fall in the range of 0.5 to 150 Hz, and filters designed to remove noise outside of that range—at the high or low end—are relatively straightforward. The process gets trickier when the interference overlaps with the ECG frequency range.
Over the years, the American Heart Association (AHA), the American College of Cardiology (ACC), and other groups have published recommendations regarding ECG measurement. In 1990, the AHA released recommendations for standardization and specifications in automated ECG, touching on issues of bandwidth and digital signal processing.1 In 1992, the AHA and the ACC issued more-comprehensive ECG guidelines.2 Then, in 2007, the AHA, ACC, and Heart Rhythm Society released updated recommendations on the standardization and interpretation of the ECG.3
Looking beyond the U.S., while the European Society of Cardiology does not have specific guidelines geared toward general ECG measurement, the group has released guidance on interpretation of neonatal electrocardiograms and on ECG interpretation in athletes (first in 2005 and then with an update in 2010).4,5,6 In 2017, an international group of experts updated the athlete-specific recommendations.7
All of these documents remain essential resources for clinicians seeking to better understand all aspects of the ECG, including the need for filtering.
There are many types of filters, but four of the most commonly used are low-pass, high-pass, power line, and anti-aliasing filters.
Low-Pass Filters
Low-pass filters allow lower-frequency signals to pass through and block any frequencies above a certain threshold, which is typically set at 150 Hz because the clinically relevant info in the ECG falls below that. If there's noise within the ECG frequency range coming from a muscle artifact or the environment, however, you can lower the cutoff accordingly.
This type of filtering will smooth out the ECG signal, easing the reader's task for interpreting findings in the lower-frequency range, like arrhythmias and QRS intervals. But it may also have an impact on the amplitude of the signal, potentially affecting the diagnosis of conditions that rely on QRS amplitude, such as hypertrophic cardiomyopathies. The lower the cutoff employed for the low-pass filter, the greater the distortion of the amplitude.
High-Pass Filters
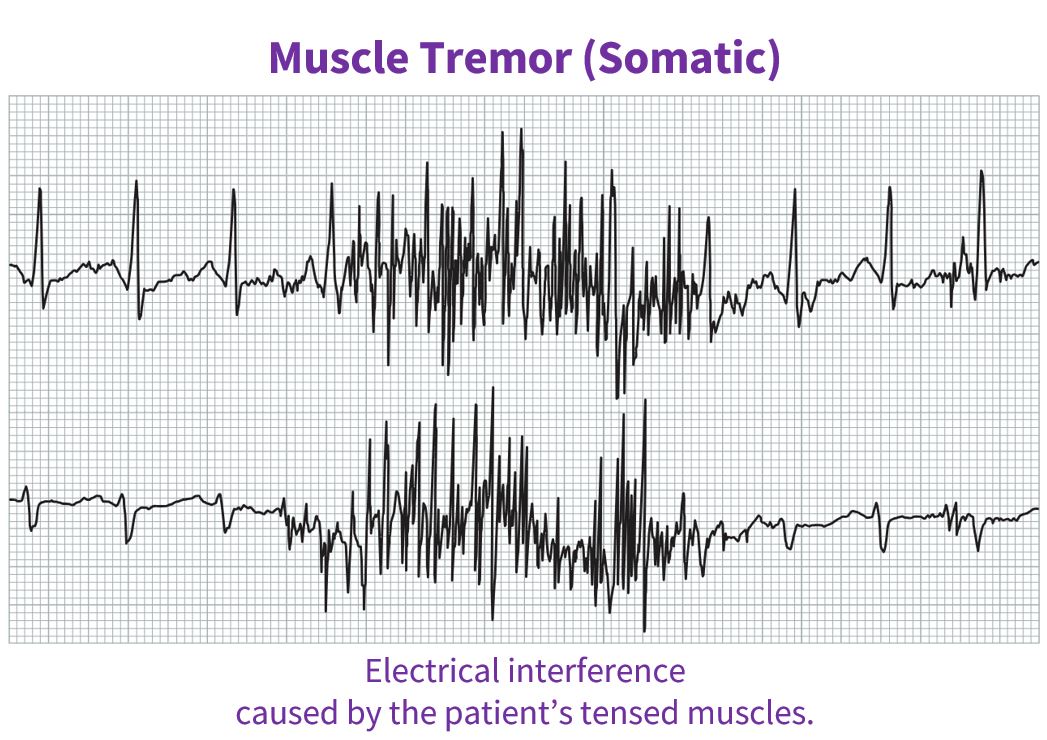
Another type of contamination you might see on the ECG is baseline wander. This is often due to the patient's breathing. If there's not a good electrical connection, this would present as a rolling of the signal on the baseline. Respiration artifacts come in below 0.5 Hz and a clinician can address them with the use of high-pass filters, which block frequencies below a specific cut point.
This type of linear filter, however, can come with both phase and amplitude distortion on the low end of the ECG frequency range. This can result, for example, in some of the energy from a high-frequency component like the QRS bleeding into and distorting the ST segment, which may lead to false-positive findings for conditions including ischemia or myocardial infarction. Using a zero-phase delay (ZPD) filter will help mitigate the effects of phase distortion.
Power-Line Filters
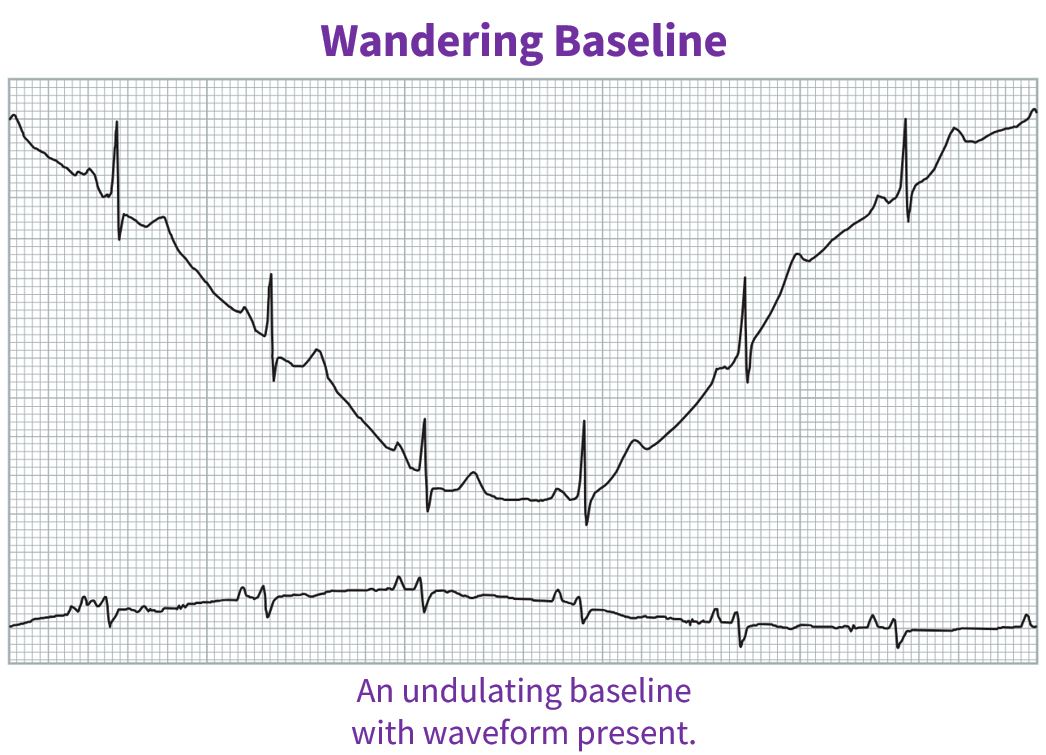
Other power sources in the environment with standard alternating current line frequencies of either 50 Hz or 60 Hz can introduce electrical noise into the ECG signal. Those can be problematic because they fall right in the middle of the standard ECG frequency range. Fluorescent lights are common sources of 60-Hz noise in the U.S.
A power-line filter will remove the fuzz in the middle of the ECG signal from these sources. These filters can effectively identify and remove this noise since it carries a specific signature. Clinicians facing this interference simply need to utilize their power-line filters for a clean ECG reading.
Anti-Aliasing Filters
A fourth common type of filter is one that performs anti-aliasing. Aliasing occurs when an analog-to-digital converter attempts conversion of a signal with a rate exceeding half of the sampling rate, which is referred to as the Nyquist frequency. This "causes portions of the displayed signal to 'fold back' on themselves and provide misleading information" and it produces "spurious information in the frequency spectrum," according to a paper in Circulation: Arrhythmia and Electrophysiology.8
If there is, for example, a cell phone sitting in the room during an ECG measurement, the signal can show up in the ECG as lower-frequency noise. A clinician can address it with an anti-aliasing, low-pass filter.
Linear vs. Nonlinear Filters
Generally, ECG filters fall within two larger umbrellas: linear and nonlinear. For linear filters, the output is a combination of the inputs. For nonlinear filters, the output is not a linear combination of the inputs.
A power-line filter serves as one example of a well-understood and necessary nonlinear filter because it addresses noise in the middle of the ECG signal frequency range. Machines can't simply remove signals at that frequency with a linear filter because doing so would eliminate important data from the ECG. Nonlinear filters can be adapted to address interference within the ECG frequency range without distorting the reading.
Still, nonlinear filters may have unpredictable effects and could distort the ECG reading if they're not working as designed. It's important for clinicians to know whether they're using nonlinear filters and how to enable or disable them if anything unusual turns up on the ECG.
Filters Should Not Be the Go-To
Of course, filtering is only necessary when other measures to ensure a high-quality ECG reading prove unsuccessful. This includes good patient preparation with proper electrode placement, the use of well-maintained and unexpired electrodes and leads, and the use of a room with an electrically controlled environment. A clean ECG should be obtainable when following best practices.
Use of filters, then, stands as the exception rather than as a convenient way to get high-quality ECG readings, given the possibility of signal distortion. In certain scenarios—when patients have Parkinson's disease or another cause of tremors, for example—filters may be unavoidable, but good patient prep should always be the first step.
Obtaining the cleanest possible ECG readings is not just critical to the best patient management. There are indications that ensuring accurate diagnoses using ECG and other testing not only improves patient care but also saves the healthcare system money.
Resources
1. Bailey JJ, Berson AS, Garson A Jr, et al. Recommendations for standardization and specifications in automated electrocardiography: bandwidth and digital signal processing. A report for health professionals by an ad hoc writing group of the Committee on Electrocardiography and Cardiac Electrophysiology of the Council on Clinical Cardiology, American Heart Association. Circulation. February 1990;81(2):730-739. https://www.ahajournals.org/doi/10.1161/01.cir.81.2.730.
2. Schlant RC, Adolph RJ, DiMarco JP, et al. Guidelines for electrocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Electrocardiography). Circulation. March 1992;85(3):1221-1228. https://www.ahajournals.org/doi/10.1161/01.cir.85.3.1221.
3. Kligfield P, Gettes LS, Bailey JJ, et al. Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society endorsed by the International Society for Computerized Electrocardiology. Journal of the American College of Cardiology. March 2007;49(10):1109-1127. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.106.180200.
4. Schwartz PJ, Garson A Jr, Paul T, et al. Guidelines for the interpretation of the neonatal electrocardiogram. A task force of the European Society of Cardiology. European Heart Journal. September 2002;23(17):1329-1344. https://academic.oup.com/eurheartj/article/23/17/1329/501315.
5. Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. European Heart Journal. March 2005;26(5):516-524. https://academic.oup.com/eurheartj/article/26/5/516/2888062.
6. Corrado D, Pelliccia A, Heinbuchel H, et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. European Heart Journal. January 2010;31(2):243-259. https://academic.oup.com/eurheartj/article/31/2/243/719826.
7. Drezner JA, Sharma S, Baggish A, et al. International criteria for electrocardiographic interpretation in athletes: Consensus statement. British Journal of Sports Medicine. May 2017;51(9):704-731. https://bjsm.bmj.com/content/51/9/704.long.
8. Venkatachalam KL, Herbrandson JE, Asirvatham SJ. Signals and signal processing for the electrophysiologist: part I: electrogram acquisition. Circulation: Arrhythmia and Electrophysiology. December 2011;4(6):965-973. https://www.ahajournals.org/doi/10.1161/CIRCEP.111.964304.