THE EFFICIENCY IMPERATIVE
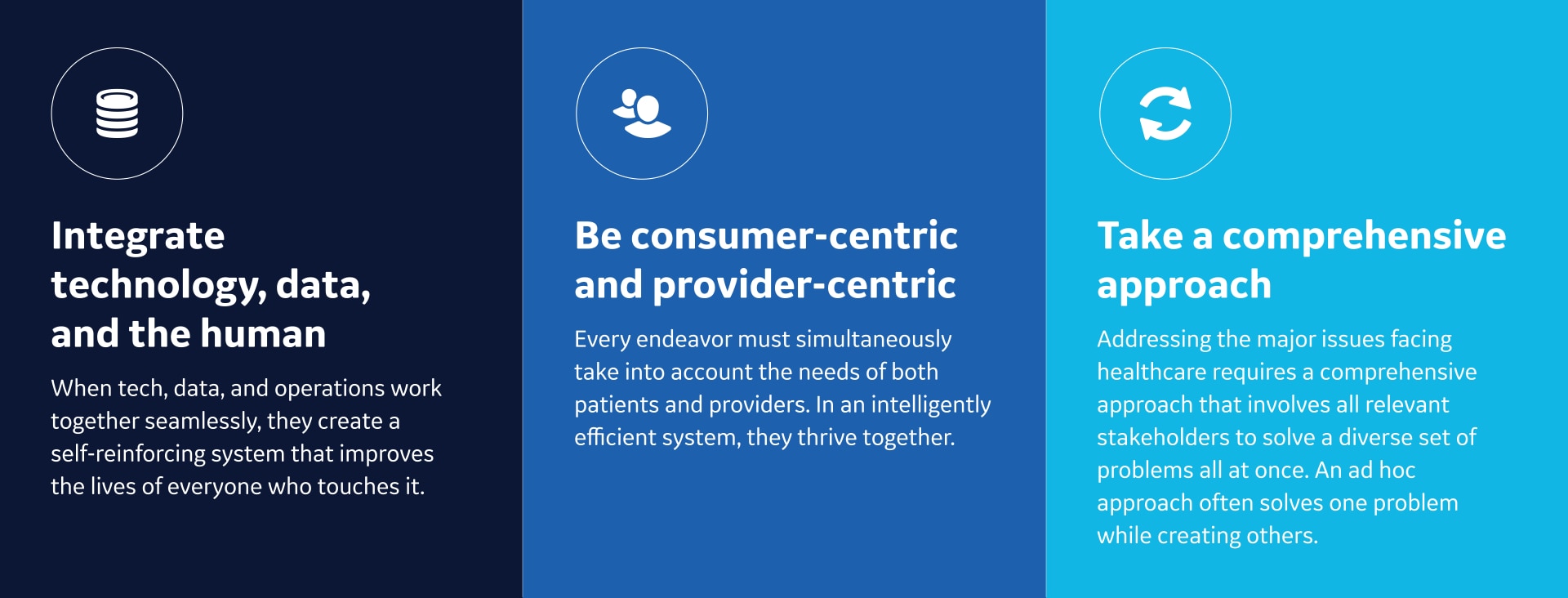
While researchers have written a great deal about the need for efficiency and productivity in healthcare, they have generally approached the issue from a purely linear, calculated standpoint. As a result, the efficiency conversation is usually dominated by a sense of value-in, value-out and a focus on how each element contributes to a very specific definition of worth. It’s worth noting that despite the attention given to efficiency much of the healthcare sector is still struggling with growing costs, greater pressure on providers, and anemic bottom lines.
But a select number of innovative institutions are charting a new path, showing that steps exist to help both individuals and institutions achieve their mission while navigating through the changing healthcare landscape. These steps are accessible to any institution, but the trick is that to successfully apply these methods, institutions will need to completely reframe their concepts like productivity, effectiveness, and efficiency. In fact, nothing short of a paradigm shift in how we view and define efficiency will be required to survive the seismic changes that characterize the contemporary healthcare sector.
AIR™ Recon DL at the Hospital for Special Surgery
The Hospital for Special Surgery (HSS) has a long history of GE collaboration in the co-development of innovative MR orthopedic solutions, such as imaging around metal implants, quantitative characterization of cartilage and nerve imaging, to name a few. Approximately 2 years ago, GE and HSS undertook a clinical evaluation study to examine a novel, deep-learning based MR reconstruction technique called
AIR™ Recon DL‡, a technique that uses GE's Edison AI Platform, trained on over 10,000 images.
During the course of this study and subsequent commercial product pilot evaluation, HSS evaluated AIR™ Recon DL and its impact on image quality, spatial resolution and acquisition scan time in peripheral nerve and musculoskeletal (MSK) imaging. The difference in enhanced image quality was “night and day,” said HSS. AIR™ Recon DL improved SNR and image sharpness when looking at musculoskeletal structures, such as ligaments, tendons, nerves and the trabecular detail of the bones. When using AIR™ Recon DL on a 512 x 512 matrix with one excitation (1 NEX), trabecular detail was not blurred, and the individual nerve fascicles were clearly demonstrated. Previously at a 512 x 512 matrix, SNR would be a significant challenge. AIR™ Recon DL also works seamlessly with AIR Touch™ workflow tools that automate the scan process to drive consistency and help facilitate shorter scan times.
With AIR™ Recon DL, HSS doctors found that they could confidently evaluate the internal architecture of the nerve — something they couldn’t routinely see before – leading to faster radiology reads and more confidence in their diagnoses established through an early adopter user survey. Ultimately that put HSS in a position to serve more patients while also producing better patient outcomes. With the accompanying new software release, HSS is now considering orthopedic protocols that are under 10 minutes or less.
‡ Not yet CE marked for 1.5T. Not available for sale in all regions.
Edison and MR Excellence Program at Robert Schumann Hospitals
Robert Schumann Hospitals in Kirchberg, Luxembourg faced a critical challenge. They needed to reduce wait time for their MR systems. The long wait times meant patients with serious pathologies were forced to delay treatment because they were not able to get a timely MR scan, and that was having a negative effect on patient outcomes and provider morale.
To help solve for this, GE Healthcare helped them integrate Edison applications into their technology and workflow. Using the MR Excellence Program to develop standardized protocols, Robert Schumann Hospitals sped up staff processes and improved reproducibly for patients with serious pathologies.
The integration was managed by a cross disciplinary team. Imaging Insights provided the data intelligence to enable better outcomes in MR, including increased patient throughput, better machine utilization, more clinical consistency, and optimal use of equipment technology. Customer enablement support brought together a team of radiologists, technologists, and department heads to help them work towards common goals.
Ultimately, this modernization and standardization turbocharged Robert Schumann Hospitals’ efficiency. The number of protocols was reduced by 47 percent. The stress on staff, particularly technicians, decreased. System utilization time went up 11 percent, with greater visibility into inactive usage windows. And, most importantly, MRI wait times were reduced by 3 weeks.
Command Centre and Imaging Tile at Humber River Hospital
With a rapidly growing community exceeding 850,000 residents, and rising ED volumes topping 400 per day, Toronto’s Humber River Hospital (HRH) determined in 2016 it would be facing a capacity shortfall of 40-50 medicine beds by the year 2020, despite the opening of a larger and digitally advanced replacement hospital in 2017. Humber River subsequently engaged GE Healthcare to establish a hospital command centre that would help enable patient flow, better patient care logistics and the delivery of high reliability healthcare.
One of Humber River’s 21 command centre analytics is the Medical Imaging Tile, which notes in real time when an ordered inpatient imaging exam remains unscheduled too long, when the order is for a critical care patient or a patient ready for discharge, or when the exam needs to be coordinated with other exams when the patient has multiple exam orders. An artificially intelligent algorithm dynamically prioritizes the queue of unscheduled inpatient exams based on a methodology provided by the hospital, and suggests optimal times during which to schedule the inpatients, accounting for the real time status of how scheduled outpatients and already scheduled inpatients are progressing. Information on the Tile is promptly actioned by the Imaging Expediter role within the command centre team. This team member, a Medical Imaging Technologist, uses their expertise and relationships with the modality teams and physicians as they work the Tile throughout the day to progress inpatient scans, reduce care delays, reduce unnecessary patient days and enable some patients to go home sooner.
Since implementing the Medical Imaging Tile, Humber River has seen a 16-27% reduction in the average time inpatients wait for medical imaging exams, depending on the modality. Inpatients are receiving a better patient experience as the Tile helps ensure they receive their exams in a timely way. Hospitalists and other caregivers are more satisfied now that they no longer need to track down contacts across the different modalities to see when their inpatients can get scanned. They now have confidence that their inpatient imaging orders are being actively managed throughout the day, intelligently, and with a level of efficiency not previously possible.
Centricity™ Cardio Workflow Connects All Diagnostic Modalities at Nuremberg Hospital
Examples of a successful efficiency mosaic can be found at Germany’s Nuremberg hospital, an institution with 2,730 beds and 6,000 staff. Feeling pressure from payors to speed up its report times for cardiology diagnostic procedures, they instituted a solution that went well beyond the cardiology department. Rather than simply conducting a training for cardiologists or adopting a one-off piece of technology that would foster faster reporting, the hospital conducted a full workflow analysis and connected all diagnostic modalities to a single cardiology information system that could generate a report available to all relevant care providers.
The effort involved adopting the Centricity Cardio Workflow system, but it also involved extensive training and education for a wide variety of hospital employees, advanced project management, and the creation of a new type of administrative report. The results reveal the benefits of this type of approach: the team decreased the time spent by cardiologists to complete cath lab reports by 60%* and increased quality control compliance to 100 percent.ii
Revolution Maxima at France Imaging Center
The leadership of a medical imaging center in Nancy, France needed to upgrade their equipment to machines that could simultaneously be used for emergency, inpatient and outpatient care, and handle wildly differing cases, including interventional imaging.
With the help of GE Healthcare, they found Revolution Maxima.
Among many capabilities, the Revolution Maxima provided them radiation dose exposure minimization, a 3D camera that analyzes the patient while lying on the table and allows technologists to detect more precisely, helping automatically identify patient scan landmark and start/end location in order to perform scout acquisition. The tablets on the gantry also enabled technologists to plan all the exam setup directly by the patient’s side for a better patient experience.
Their move from a manual CT scanner to a completely automated protocol automatically centering and positioning the patient, not only changed the way the Center works for the better, making them faster and more precise, it also left more time for the technologist to care for what matters most: the patients.
Oregon Health and Science University’s (OHSU) adopts the Mural™ Virtual Care Solution (Mural)
An example of a true holistic approach is Oregon Health and Science University’s (OHSU) adoption of the Mural™ Virtual Care Solution (Mural), a platform that integrates real time data from multiple systems and devices to paint a comprehensive picture of patient status and prioritize clinicians’ attention to the most critical patients across multiple facilities, based on hospital defined protocols. In the face of the COVID-19 pandemic, the timely adoption of Mural™ allowed the teaching hospital to operate more efficiently by enabling specialists in a central location to provide clinical support to bedside teams caring for patients in multiple ICUs.
OHSU took a system-wide approach to the adoption of Mural™, working with front line providers to ensure the solution would support their current workflows by digitizing their defined protocols and best practice standards. The result was a system that improved efficiencies in care delivery by allowing critical care experts to remotely oversee data such as patients’ vitals and best practice standards in near real time. Just as importantly, it also allowed for better visibility into ICU bed access for those in need of intensive care, better data collection and monitoring for individual patients, greater satisfaction among providers who found it easier to fulfill their mission of delivering high-quality patient care, and a more efficient distribution of hospital beds across the system.
Contact Us
vii https://www.mayoclinicproceedings.org/article/S0025-6196(19)30836-5/fulltext
viii https://www.gehealthcare.com/-/jssmedia/syneos/centricity-cardio/ge-healthcare-klinikum-nurnberg-case-study.pdf
ii https://www.gehealthcare.com/-/jssmedia/syneos/centricity-cardio/ge-healthcare-klinikum-nurnberg-case-study.pdf
