By Dr. Payal Kohli, MD, FACC
When we see another physician, we rarely see the person or perhaps even the patient that may be hiding behind their white coat. It was during a recent cardiology conference that I realized a colleague and friend of mine was more than just another noninvasive cardiologist—she was a heart disease survivor. During a lunch we shared at the conference, she opened up to tell me about her spontaneous coronary artery dissection during her cardiology fellowship training. She shared how she experienced nausea while on rounds and used the ECG function on her smartwatch to self-diagnose ST elevation, which resulted in a lifesaving trip to the cath lab for her at the young age of 34 years.
Her story gave me a newfound respect for the electrocardiogram. Even for the most highly trained observer (a cardiologist), who is accustomed to dealing with heart disease every single day and highly attuned to the signs and symptoms, the 12-lead ECG is a fundamental and necessary diagnostic tool. It can literally establish the difference between life and death—between an emergency or a less acute situation. The electrocardiogram saved her life that day. Had she not obtained that single-lead ECG, and had we not rushed her to the cath lab, her prognosis may have been completely different.
This got me wondering about what would have happened if she had sustained a dissection of her right coronary artery and the single-lead ECG from her wrist (lead I) had been unrevealing. Would she have followed up with a 12-lead ECG? Had she just looked at a single lead (and if her dissection involved a coronary artery that was not represented on that lead), she may have had a falsely negative reassuring result. A study in the Journal of the American Medical Association Cardiology showed that the smartwatch could be placed on different parts of the body to obtain a multi-channel ECG, and these correlated well with standard ECGs for the identification of acute coronary syndrome.1
I had recently seen a presentation on an 80-lead 3D ECG "vest" that could be placed on patients and provide a three-dimensional 360-degree view electrical map of the heart with greater sensitivity and comparable specificity in detecting acute myocardial infarction (AMI) compared to the 12-lead ECGs.2 This required minimal training on the part of the healthcare provider seeing as the computer-synthesized diagnosis localized the culprit vessel and also accounted for confounding factors, such as left bundle branch block, left ventricular hypertrophy, and early repolarization.
So, what is the right "number" of ECG leads then? Do more leads equal better care? If so, what are the situations to use more leads, and how do more leads affect the clinical care of patients?
Diagnostic Accuracy
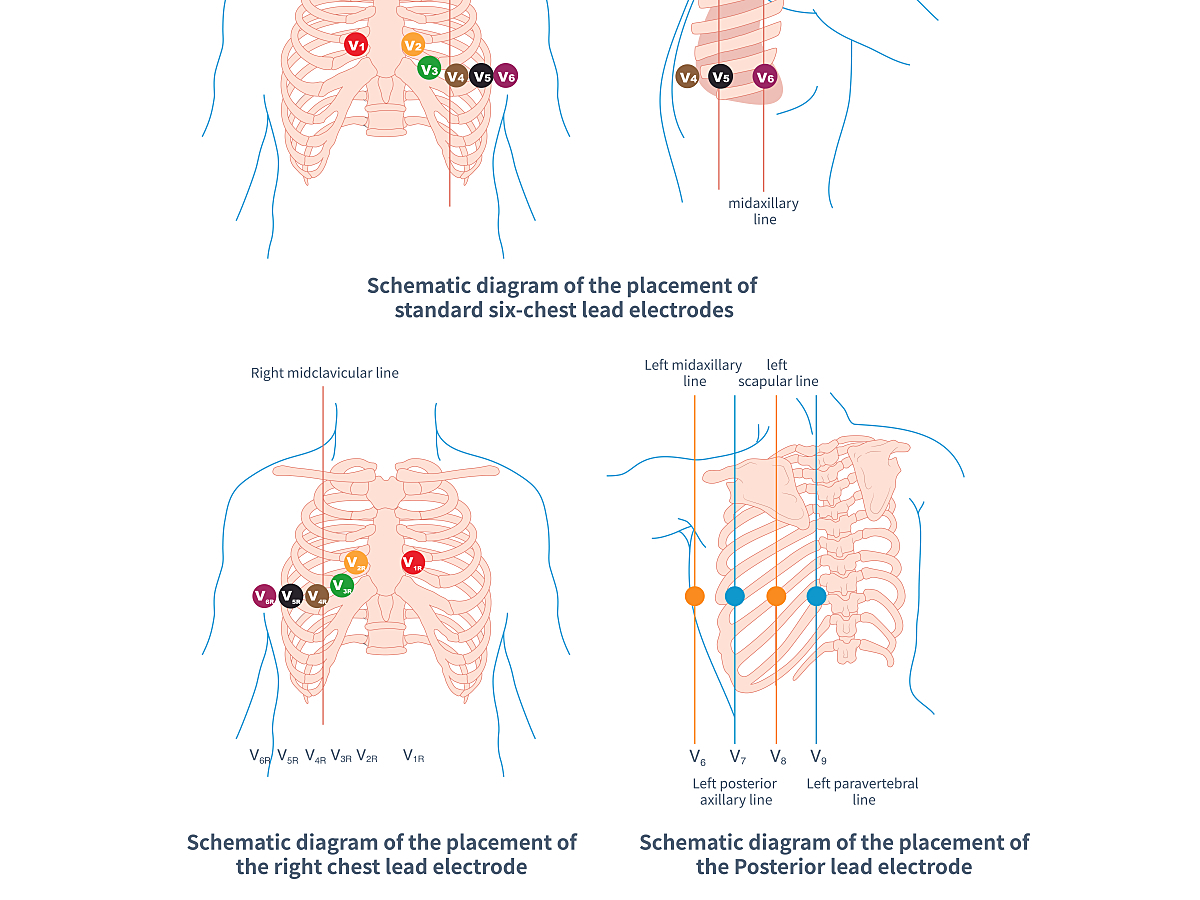
It is known that the traditional 12-lead can be more limited when it comes to certain types of AMI. An American Heart Association Scientific statement reports that recordings from right-sided and posterior ECG leads increases the diagnostic sensitivity for STEMI.3 However, additional leads required electrode repositioning and a change in patient positioning to obtain V3R-V6R and V7-V9. For this reason and others, they are not routinely done in clinical practice.
The classic "must not miss" diagnosis is the true posterior ST-elevation myocardial infarction (MI), which appears on every board exam and usually presents with anterior ST-segment depressions (representative of posterior wall ST-segment elevations). In such cases, leads V7-9 are added to the traditional 12-lead. Seeing as the infero-posterior wall can receive its blood supply from a posterior descending artery originating off the right coronary artery (right dominant) or the left circumflex artery (left dominant) or both (co-dominant), assessment of right-sided leads is also important with V4R-V6R. Such a diagnosis is critical because it can affect hemodynamic management as well as the decision to use nitrates during the acute presentation.
So, this begs the question of whether an 18-lead ECG (standard 12-leads plus V7-V9 and V3R-V5R) or a 15-lead (standard 12-leads plus V8-V9 and V4R) should become standard in practice.
The 18-lead and 12-lead approaches were compared in a study published in the American Journal of Cardiology and reported that posterior and right-ventricular leads increased the sensitivity for AMI by 8.4% but decreased the specificity by 7%.4 Four leads (I, II, V3, and V5R) were independently predictive of AMI. Therefore, despite its limitations, the diagnostic accuracy of the standard 12-lead was improved but only modestly and with a tradeoff in reduced specificity. However, in another study published in The Annals of Emergency Medicine, the 15-lead ECG provided increased sensitivity and odds of detecting ST-segment elevation in AMI with no loss of specificity.5 Similar findings were reported in another prospective study in the American Journal of Emergency Medicine.6
Infarct Localization
Certainly, routinely obtaining additional leads could more rapidly aid in the diagnosis and localization of posterior or right-ventricular infarcts.7 Although modern management of acute ST-elevation MI mandates a trip to the cath lab (when revascularization facilities are available), more accurate localization of the culprit vessel may help to improve door-to-balloon times in injection, localization, and intervention of the vessel first. Thus, the application of the 15-lead ECG may be most appropriate in a triage emergency room setting, with less relevance in routine outpatient testing or electrophysiology clinics.
Guidelines from The American College of Cardiology /American Heart Association Task Force on Clinical Practice as well as the European Society of Cardiology recommend that patients with inferior ST-elevations (AMI with ST elevation in II, aVF, or III) and hemodynamic compromise be assessed; a right precordial lead (V3R and/or V4R) should be added to detect whether there is right ventricular infarction or involvement.8
Training and Interpretation
Before the 15-lead or 18-lead ECG is routinely incorporated into clinical practice, however, additional considerations would have to account for further training of healthcare providers to interpret this expanded diagnostic testing. A meta-analysis published in the Journal of the American Medical Association Internal Medicine suggests that physicians at all training levels have deficiencies in 12-lead ECG interpretation—and although this improved after training, the overall accuracy was still relatively low.9
Beyond 12 Leads?
The 12-lead ECG continues to remain the gold standard for diagnosis of AMI, and there doesn't appear to be a "magic" number of leads that is universally recommended for this diagnosis. However, selective use of expanded 15-lead or 18-lead ECGs has a definitive clinical role in improving the sensitivity of diagnosis and should be utilized in triage or emergency room settings and, per the guidelines, in situations with inferior ST-segment elevation. If it's utilized in such settings, additional training for healthcare providers should be mandatory to ensure accurate interpretation.
My colleague was lucky that her single-lead ECG identified her AMI because it's known that fewer leads have significantly lower sensitivity for the detection of MI.
Resources:
- Spaccarotella CAM, Polimeni A, Migliarino S, et al. Multichannel Electrocardiograms Obtained by a Smartwatch for the Diagnosis of ST-Segment Changes. JAMA Cardiology. 2020;5(10):1176–1180. https://jamanetwork.com/journals/jamacardiology/fullarticle/2770022
- Cision PR Newswire. Verathon® introduces the Heartscape™ 3D ECG system with 80-lead vest in Europe; Technology provides more complete data to help diagnose acute myocardial infarction (MI). PRNewswire.com. Accessed January 9, 2023. https://www.prnewswire.com/news-releases/verathon-introduces-the-heartscape-3d-ecg-system-with-80-lead-vest-in-europe-technology-provides-more-complete-data-to-help-diagnose-acute-myocardial-infarction-mi-128060878.html.
- Amsterdam EA, Kirk JD, Bluemke DA, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association.Circulation. 2010;122:1756–1776. https://doi.org/10.1161/CIR.0b013e3181ec61df.
- Zalenski RJ, Rydman RJ, Sloan EP, et al. Value of posterior and right ventricular leads in comparison to the standard 12-lead electrocardiogram in evaluation of ST-segment elevation in suspected acute myocardial infarction. American Journal of Cardiology. 1997;79(12):1579-85. https://doi.org/10.1016/S0002-9149(97)00202-6.
- Zalenski RJ, Cooke D, Rydman R, et al. Assessing the diagnostic value of an ECG containing leads V4R, V8, and V9: The 15-Lead ECG. Annals of Emergency Medicine. 1993; 22:(5):786-793. https://doi.org/10.1016/S0196-0644(05)80792-9.
- Brady WJ, Hwang V, Sullivan R, et al. A comparison of 12- and 15-lead ECGs in ED chest pain patients: impact on diagnosis, therapy, and disposition. Am J Emerg Med. 2000;18(3):239-43. https://doi.org/10.1016/S0735-6757(00)90112-8.
- Ashida T, Tani S, Nagao K, Yagi T, et al. Usefulness of synthesized 18-lead electrocardiography in the diagnosis of ST-elevation myocardial infarction: A pilot study. American Journal of Emergency Medicine. 2017;35(3):448-457. doi: 10.1016/j.ajem.2016.11.052. https://doi.org/10.1016/j.ajem.2016.11.052.
- Antman EM, Anbe DT, Armstrong PW, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004;110(5):588-636. https://doi.org/10.1161/01.CIR.0000134791.68010.FA.
- Cook DA, Oh SY, Pusic MV. Accuracy of physicians' electrocardiogram interpretations: a systematic review and meta-analysis. JAMA Internal Medicine. 2020;180(11):1461-1471. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2771093.
Dr. Payal Kohli, MD, FACC is a top graduate of MIT and Harvard Medical School (magna cum laude) and, as a practicing noninvasive cardiologist, is the managing partner of Cherry Creek Heart in Denver, Colorado.
The opinions, beliefs, and viewpoints expressed in this article are solely those of the author and do not necessarily reflect the opinions, beliefs, and viewpoints of GE Healthcare. The author is a paid consultant for GE Healthcare and was compensated for creation of this article.