In medical school, physicians-to-be get a crash course on pretty much every aspect of medicine, including ECG. By the time they take their board certifications, they likely have a good enough handle on the tool to pass standard tests, such as identifying Afib or STEMI.
But that training leaves some gaps regarding the nuances of ECG, such as electrode placement, abnormality detection, and changes over time. Understanding these and other subtleties can inform immediate clinical decision-making, but if physicians aren't sufficiently trained on ECG, it can put them and their patients at a disadvantage.
So says Anthony Kashou, MD, a global expert known as "The EKG Guy." He suggests that all clinicians take steps to study basic and advanced applications of electrocardiography. After all, the tool offers something for everyone, including non-cardiologists.
"It's difficult to imagine something more central to the practice of medicine than the performance and interpretation of the ECG," he said. "It's a simple, rapid, and noninvasive diagnostic test and remains an important aspect of patient care across a variety of settings and specialties."
We talked with Dr. Kashou to understand why ECG is so critical in any care area, and how clinicians can get up to speed with its many nuances.
A Tool That Stands the Test of Time
It's been more than a century since ECG's earliest iterations, and the tool has undergone a renaissance of changes that have made it more powerful and accessible to clinicians and patients.
"This evolution is occurring both at the software level and the hardware level," Dr. Kashou said. "We're seeing artificial intelligence techniques such as machine learning and deep learning models that are giving way to opportunities to see beyond what the human eye can see. And meanwhile, patients are also getting the opportunity to record ECG from home with new devices that are coming to the market."
Despite these innovations, ECG still does what it always has: It measures the electrical signals of the heart, spotting irregularities that can determine when something's wrong. That's what makes this device stand the test of time, even in non-cardiology care areas.
"It's way more than just cardiologists who will encounter ECG in their practice," Dr. Kashou said. "There are EMS, emergency physicians, critical care providers, nurses, anesthesiologists—the list goes on and on. These are people who are on the front lines who use the ECG to triage appropriate care for patients."
ECG also has utility in outpatient settings such as primary care. If, for example, your patient came in with palpitations, you'd run an ECG, as is the standard.1 If the ECG indicates Afib, it might warrant anticoagulation to reduce stroke risk. In this instance and others—including providing care to COVID-19 patients—ECG can change care management in real time.
The Learning Curves of ECG
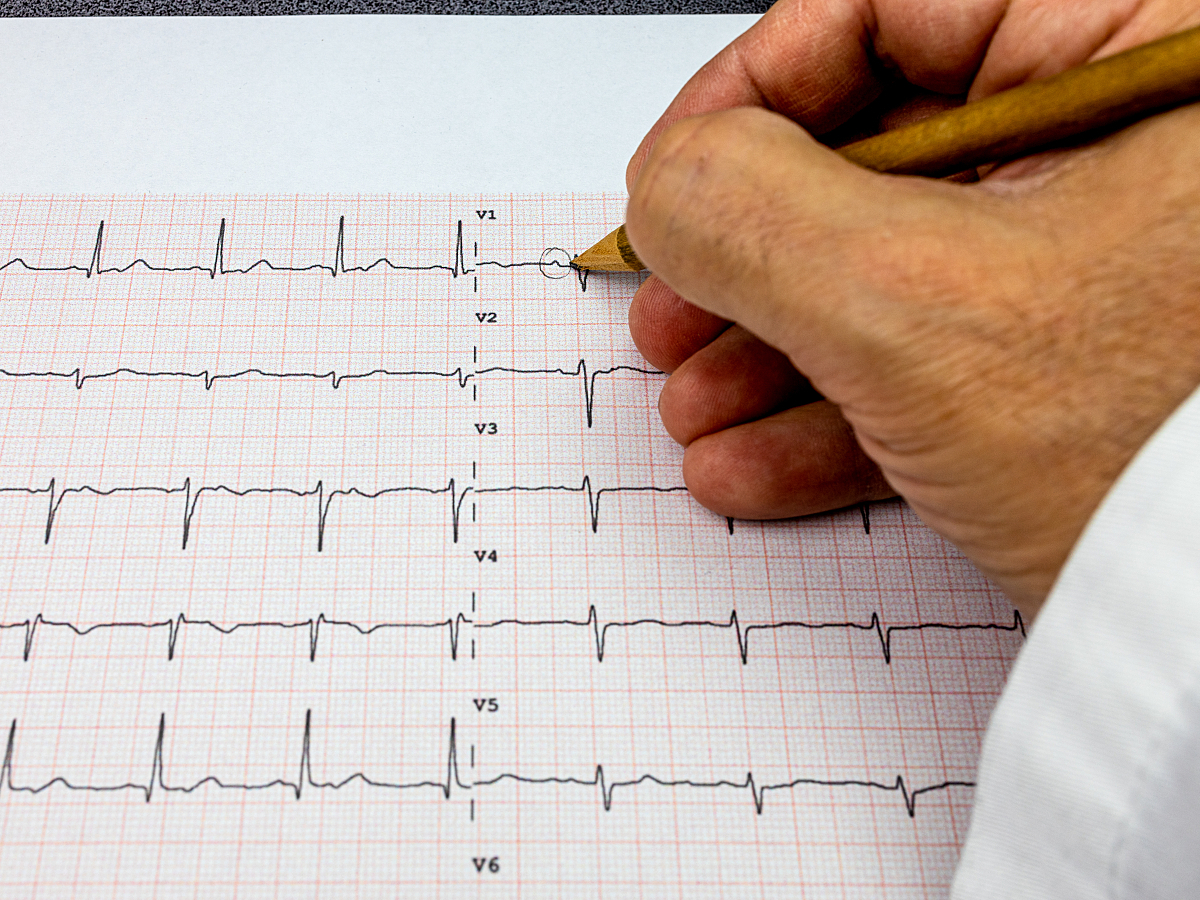
Diagnostically important as it may be, ECG is also difficult to learn. Its diverse mix of peaks, valleys, distances between events, and other structural attributes can make it hard to keep up, and as a result, some clinicians may feel trepidatious about using it.
"ECG interpretation is a challenging cognitive skill set that demands a considerable amount of time and effort to develop," Dr. Kashou said. "Novice operators may mistakenly believe that electrocardiography simply boils down to memorizing a bunch of patterns, rules, or intricate characteristics that define a specific heart rhythm or cardiovascular condition."
But that's not what ECG interpretation is or should be, he adds. Rather than memorizing what problems look like, interpreters should first consider what a normal ECG reading is—waves, intervals, segments, QRS complex, and all. In a recent webinar with GE Healthcare, Dr. Kashou did just that step-by-step.
Once clinicians understand these basic components, along with the patient's clinical context, they can then start to see how deviations from those normal waveforms can indicate clinical concerns.
Many physicians might quickly recognize the clear ST-elevation pattern resembling an acute myocardial infarction. However, identifying more subtle patterns with similar underlying pathophysiology can be difficult. In such cases, a trained eye can benefit patient care.
Specialized Training for Faster ECG Learning
How can clinicians overcome the learning gaps to become more proficient users and interpreters of ECG? That's the million-dollar question, says Dr. Kashou. While there's no shortage of learning tools out there, the industry doesn't yet have a good handle on which ones work best.
Together with his team and partners, including the Mayo Clinic and GE Healthcare, Dr. Kashou aims to answer those unsolved questions with the multi-institution EDUCATE (Education and Curriculum Assessment for Teaching Electrocardiography) trial.
"We're really looking at the efficacy of using various online active learning approaches for improving ECG interpretation competency," he said. "And we're doing this across many different specialties, training levels, and disciplines."
Until that trial yields results, however, novice learners have several reputable options to expand their ECG competencies. Manufacturer-offered education is one option. Dr. Kashou also offers many learning tools on his website for use by multidisciplinary ECG operators.
To learn more about the power of the ECG in today's clinical landscape, browse our Diagnostic ECG Clinical Insights Center.
Technologies That Automate ECG Interpretation
ECG users don't have to self-learn everything; sometimes, technology can help. In particular, computerized and automated interpretations have made ECG platforms more practical for users of all experience levels, Dr. Kashou explains.
"The computer plays a tremendous role in our clinical practice," he said. "In fact, it's often the initial interpretation available when an ECG is recorded."
Generally, the aims of these technologies are three-fold: 1) to supplement clinicians' competencies, 2) to minimize medical errors, and 3) to make clinical workflows more efficient. The combination of all three makes computerized interpretation a more functional aspect of modern-day care delivery.
Even so, these technologies aren't a panacea, and they can't replace human expertise or the need to train on ECG, at least for now. Rather, computerized interpretations should be considered a supplementary resource that can get clinicians up to speed with this powerful technology.
"We don't want a tool to ever replace clinical judgment," Dr. Kashou said, adding that computerized interpretations will also be a studied endpoint of his team's EDUCATE trial. "But we're excited to see what benefits these automations bring. I think we'll see that they do deliver a lot of value to everyday ECG practice."
Making ECG More Accessible to All
As Dr. Kashou emphasizes, ECG isn't an easy tool for beginners to learn; it takes time and ample practice. But with the benefits that ECG provides in real-time clinical decision-making, the effort is well worth it.
"Learning ECG is a lifelong journey," he said. "But if you do take the time to learn how to become comfortable interpreting ECGs independently, you will be a tremendous asset on any clinical team, and you might even save a patient's life."
References
- Goyal A, Robinson KJ, Katta S, Sanchack KE. Palpitation. NIHx.gov. https://www.ncbi.nlm.nih.gov/books/NBK436016/. Accessed August 10, 2022.
The opinions, beliefs and viewpoints expressed in this article are solely those of the author and do not necessarily reflect the opinions, beliefs and viewpoints of GE Healthcare. The author is a paid consultant for GE Healthcare and was compensated for creation of this article.